A Cloud Telemedicine Platform Based on Workflow Management System: A Review of an Italian Case Study
Volume 7, Issue 6, Page No 87-102, 2022
Author’s Name: Gianvito Mitrano1,a), Antonio Caforio2, Tobia Calogiuri1, Chiara Colucci3, Luca Mainetti1, Roberto Paiano1, Claudio Pascarelli1
View Affiliations
1University of Salento, Department of Engineering for Innovation, Via per Monteroni, Lecce, 73100, Italy
2A-thon s.r.l., Via dei Tufi 4, Monteroni di Lecce (Le), 73047, Italy
3National Interuniversity Consortium for Informatics, Via Ariosto 25, Roma, 00185, Italy
a)whom correspondence should be addressed. E-mail: gianvito.mitrano@unisalento.it
Adv. Sci. Technol. Eng. Syst. J. 7(6), 87-102 (2022); ![]() DOI: 10.25046/aj070610
DOI: 10.25046/aj070610
Keywords: Telemedicine, Teleconsultation, Telemonitoring, Business Process Management, Workflow Management System
Export Citations
The paper aims to describe a new technological and organizational approach in order to manage teleconsultation and telemonitoring processes involving a Physician, who remotely interacts with one or more Specialists, in order to evaluate and discuss the specific clinical conditions of a patient, based primarily on the sharing of digital clinical data, reports and diagnostic images. In the HINT project (Healthcare INtegration in Telemedicine), a teleconsultation and telemonitoring cloud platform has been developed using a Hub and Spoke architecture, based on a Business Process Management System (BPMS). The specialized clinical centres (Hubs) operate in connection with the territorial hospital centres (Spokes), which receive specific diagnostic consultations and telemonitoring data from the appropriate Specialist, supported by advanced AI systems. The developed platform overcomes the concepts of a traditional and fragmented teleconsultation and consequently the static organization of Hubs and Spokes, evolving towards an integrated clinical workflow management. The project platform adopts international healthcare standards, such as HL7 FHIR, IHE (XDS and XDW) and DICOM for the acquisition and management of healthcare data and diagnostic images. A Workflow Management System implemented in the platform allows to manage multiple and contemporaneous processes through a single platform, correctly associating the tasks to the Physicians responsible for their execution, monitoring the status of the health activities and managing possible clinical issues.
Received: 27 July 2022, Accepted: 16 October 2022, Published Online: 26 November 2022
1. Introduction
This paper is an extension of work originally presented in the 10th International Conference on Information Systems and Technologies (ICIST 2020) entitled “HINT project: a BPM teleconsultation and telemonitoring platform” [1]. It is focused on the implementation of a telemedicine (teleconsultation and telemonitoring) platform, based on diagnostic imagines, which supports the Hub and Spoke clinical model.
In particular, optimized teleconsultation processes, supported by proper technological infrastructures, allow: i) to share data and diagnostic images between several professionals; ii) to have the first or second opinion evaluations in a very short time; iii) to prevent the patient from moving between Physicians for consultations; iv) to provide precise evaluations and diagnoses to the patient by reducing waiting times. Moreover, telemonitoring allows to control the specific vital parameters of each patient and to manage alerts if necessary [2], [3].
Over the years, many definitions of telemedicine have been given, based on the use of IT (Information and Telecommunication Systems) for remote clinical data exchange between the medical team (Physician, Nurses, Specialist) and patients, in order to provide the remote healthcare treatment. Some of these definitions are given below.
The American Telemedicine Association gives a definition of telemedicine as “The use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status” [4].
The World Health Organization (WHO) defines telemedicine as follows: “The delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of diseases and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities” [5].
The outcomes of telemedicine services can be: i) accessibility to healthcare in remote areas, allowing consistent and reliable communication; ii) fast, affordable, and reachable care; iii) h24 diagnosis (also known as night-hawking); iv) efficiency in care delivery like telestroke scenario; v) cost and time optimization and saving; vi) better collaboration between Specialists [6].
Telemedicine can also reduce the risk of hospitalization, thanks to its ability to decrease in-clinic visits, promoting remote services for patients [7]. Another important outcome can be a more effective patient engagement and evolvement, which could help users to be informed overtime about their care plan and become more aware of their health. Telemedicine can also represent an effective way to treat depression and other mental health conditions, helping patients with mental disorders unwilling to seek any treatment in normal circumstances, and making use of video or remote controls.
Telemedicine services can be divided into synchronous and asynchronous services. In the former case, the service establishes an interaction and connection in real time (through audio or video-conferencing technologies) between the parties requiring their presence at the same time; in the latter case, clinical and medical data are temporarily stored and later transmitted to the Physician or medical Specialist for an offline assessment. Synchronous telehealth models can help to provide timely care, especially for emergency care or urgent situations. On the other hand, asynchronous models are ideal for evidence-based and not emergency care [8].
In healthcare, especially in telemedicine, some fundamental aspects concern the quality of data, clinical documents, diagnostic images and the modality to exchange. Physicians and healthcare professionals need to access and share all the patient’s information and clinical data, also deriving from telemonitoring activities, and it is, therefore, necessary the interconnection between different Information Systems and the consequent interoperability based on clear and possibly open rules and standards [9], [10].
Interconnected and interoperable systems are defined as integrated if, thanks to the use of standard languages, protocols and formats, they allow to define the methods of transmission and reception of data, as well as their representation (syntax) and their semantics [11].
In the healthcare sector, there are several models and open standards for the information and clinical data management and exchange, among which, for the best of authors’ knowledge, the most widely used are IHE (Integrating the Healthcare Enterprise), DICOM (Digital Imaging and Communications in Medicine) and HL7 (Health Level Seven) for the diagnostic images sharing [12].
These standards are used in order to have an effective interoperability between the Health Information Systems (HIS)such as hospital RIS (Radiology Information System), PACS (Picture Archiving and Communication System) and booking centers (e.g., the Italian CUP) [13].
Alongside the standards and new healthcare information technologies mentioned above, it is important to define and optimize clinical processes through the use of management approaches such as the BPM (Business Process Management), which allows to model, define, organize, execute and monitor the clinical activities of interest.
In this paper, after an initial overview of the motivation behind this work, section two provides a narrative literature review about telemonitoring and teleconsultation applications. The third section describes the HINT project, that has developed a cloud platform based on a Hub and Spoke architecture where telemedicine processes are managed by a BPM workflow system. The fourth section illustrates these processes modelled through the BPMN notation, with a detailed analysis of the following scenarios: Neuro-Radiological Teleconsultation, Dermatological Teleconsultation and Obstructive Sleep Apnoea Syndrome Telemonitoring. Finally, discussion and conclusions close the paper.
1.1 Motivation
Different telemedicine projects propose generic solutions with static Hub and Spoke architecture [14], [15], in which the teleconsultation and the exchange of clinical data and information take place through traditional clinical assessment, in absence of a single management platform and digitalized telemedicine pathways for the real time sharing of reports, diagnostic images and documents. To overcome a typical static organization, the HINT project envisages the use of a workflow engine for the complete routing and management of the consultation request and parameter monitoring to the appropriate and available Hub.
Moreover, the Hub Specialist can be helped in his/her clinic evaluation by Decision Support Systems (DSSs) based on Deep Learning, which can analyse and classify dermatological images and to manage out-of-threshold values with alerts. Specifically, the project proposal is an advanced teleconsultation and telemonitoring system, in which Physicians can: i) receive technological support through DSSs; ii) are aware of the consulting request status in every moment and iii) provide detailed clinical information to make assessments and final diagnoses. The HINT Hub and Spoke system allows the identification of the most appropriate available Specialist for the dermatological case to be treated, who responds on a single, integrated platform with his/her second opinion evaluations. It is particularly valuable in all the cases requiring high healthcare specializations, especially in remote areas where they are not immediately available.
Furthermore, the HINT platform wants to guarantee timely and constant monitoring of specific vital parameters in the treatment of sleep apnoea through UWB devices. It is supported by the implementation of a Workflow Management System for healthcare process digitalization through the application of the IHE standard (XDW) for the definition and traceability of all the steps, actors and documents produced in the clinical care processes.
2. Literature review
In this section, a literature study is carried out to analyse the different telemedicine services implemented in the HINT system, which are teleradiology, teleconsultation and telemonitoring. A review on information systems and standards is also provided.
Teleradiology is implemented in different countries in order to face the following issues [1], [16]:
- out-of-hour coverage by means of intramural services (at-home control);
- out-of-hour coverage by means of extramural services;
- rural or regional hospital coverage;
- Specialist’s second opinion.
In [16], the authors summarize some of the key aspects in image acquisition, transmission, and interpretation, with a discussion of the clinical practice of teleradiology.
A survey [17] states that 44% of the European radiologists use at-home control instead of call referral. In many cases this procedure is not based on a structured Hub and Spoke architecture, but only on the diagnostic image transmission to the Radiologist who sends the referral to the Physician by email or phone (79% of the cases).
It is also important to mention the Kaiser Permanente hospital [18] where, during the out-of-hours, there are only 2 radiologists sending medical reports for 11 different image acquisition sites, instead of having a specific Radiologist, called when needed, in each hospital.
In the U.S., it is estimated that over than 50% of the hospitals use out-of-hours reporting or night-hawking [19]. It is possible to gain an advantage from the different time zones by using extramural services. For example, in [20] radiologists from Sydney are called by a Swedish hospital for emergency; while in [21] an American hospital requests a consultation to radiologists located in India. Moreover, in [22] the authors report that radiology delays are shorter when teleradiology is used [1].
In [23], the authors delineate the main reasons for the medical imaging demand growing in Europe and U.S., explaining why teleradiology is critical to support this development in Europe. In particular, the paper presents three different teleradiology case studies regarding successful data sharing and innovative workflow models through single imaging implementations.
Furthermore, radiology is becoming increasingly specialised in recent years. The studies [24], [25] illustrate the improvement associated with producing a subspecialist report compared to a general one. In this context, teleradiology can be used to gain access to radiologists who are well trained in a particular field. Regarding this aspect, [26] underlines that teleradiology is an important component in radiology field for many aspects, one of which is the possibility to facilitate seeking a second opinion from an expert, improving in this way the efficiency and effectiveness of healthcare system. In particular, the paper presents a model based on second opinion teleradiology consultation service, which involves an Israel health insurance company and a premier medical center in San Francisco, showing in detail the operational procedure of this second opinion service [26].
In [27], the authors state that fast wireless network and mobile technologies allow to evaluate diagnostic images with a comparable accuracy to PACS workstations. In [28], the authors design and develop an economic web based platform for the diagnostic images referral by means of IT technologies. For more details about this approach, [29] gives a complete historical overview of the applications in the teleradiology sector [1].
Moreover, the tele-imaging application represents a significant chance for the future and it is a central practice for telemedicine. In particular, it includes the transmission of medical digital images and has an important role in all fields of telemedicine, such as expertise, consultation, teaching and research activities [30].
Another field of tele-imaging concerns teleconsultation, whose overall goal is to overlook geographical and functional distance between two or more geographically separated healthcare providers, using information and communication technology [31]. Surgery and general medicine are among the most common topics in adult teleconsultations. In particular, surgery teleconsultations are generally performed by sending radiology images (teleradiology), clinical pictures or videos, in order to reduce unnecessary patient transfers or travels with related costs, and also to support prompt decision making with high diagnostic accuracy, improving the future of the healthcare delivery [31].
In this context, teleconsultation is increasingly becoming an integral part of the hospital procedures. A European survey [14] estimates that 65% of all radiologists currently use teleradiology for the images sharing within the organisation and for on-call readings from home [32].
Moreover, some hospitals, especially in the United States, use teleconsultation to manage out-of-hour reporting by adopting a complete Hub and Spoke architecture. The architecture involves configurations which are centers of excellence opened 24 hours a day, providing highly complex diagnostic-therapeutic services (Hubs), and other configurations which aim to create a territorial network of services for the management of patients once overcome a certain clinical severity threshold (Spoke) [1], [33].
Additionally, teleconsultation is also applied in emergency or urgent situations, for example during pre-hospital critical care situations [34] or for emergency orthopaedic patients by mobile phone messages [35] or even for ophthalmic emergency consultation, through the use of a smartphone App or PC and a webcam [36].
There are also many studies about telemonitoring application; in particular, an analysis presented in [37] and conducted on 65 studies in the field of telemonitoring for cardiovascular, pulmonary, hypertension and diabetes diseases, describes the maturity and reliability of remote monitoring technologies [1]. Telemonitoring has also demonstrated the ability to identify changes in the condition of chronic patients at an early stage of their disease, obtaining fast intervention and avoiding complications [31]. An example is reported in [38], which refers to diabetic patients affected by a reduction in haemoglobin A1c and a significant blood glucose increase. For patients affected by hypertension, [39] reports how to respond through telemonitoring to a systolic and diastolic blood pressure reduction. In [40], [41], the authors report a high level of satisfaction of telemonitoring processes and [42], [43] emphasize the positive contribution given by telemonitoring to the decrease of hospital admissions for heart and pulmonary diseases.
Through telemonitoring it is also possible to analyse the Continuous Positive Airway Pressure (CPAP) in patients with Obstructive Sleep Apnoea (OSA) [44]. In particular, a study [45] based on [46], [47], shows that CPAP compliance is significantly higher in the Telemonitor (TM) care group compared with the usual care group, thanks to current technological advances and to the use of innovative medical devices which allow patients to control some vital parameters at home.
Telemonitoring is also applicable in the cardiology sector, for example through the development of a phone-based and rule-based expert system for heart failure telemonitoring, designed to provide remote clinical support for patients with cardiological problems [48], [49]. Another important field of application of telemonitoring concerns the control of elderly people [1], [50].
A complete review of telemedicine, is proposed into [51], which contains detailed information about: telecardiology, telestroke, teleradiology, teleoncology, teledermatology, telepathology and telemonitoring.
2.1 Health information systems and standards
An Information System (IS) can be defined as a technical and organizational system designed to collect, process, store, and exchange information and data [52].
In healthcare organizations (i.e. hospitals, radiology departments), IS manages all clinical data, diagnostic images, and reports. HIS (Hospital Information System), RIS (Radiology Information System), PACS (Picture Archiving and Communication System) are some of the most important clinical Information Systems applied in healthcare organizations [53], [54]:
- HIS: system based on IT used in healthcare to manage the administrative and clinical flows of a hospital;
- RIS: system used to manage the radiology data flow, with the purpose to collect, manage and display data and information produced in the Radiology Department;
- PACS: system used for archiving images acquired from modalities applications, managing worklists, and accessing images from reporting stations (workstations) [55].
The RIS is a HIS subsystem, while the PACS, an independent system integrated with the others, deals with the diagnostic images management.
The integration among the different systems and, in particular, between the RIS and the PACS within Radiology Department should lead to: i) use a single medical registry; ii) have a simultaneous display of images and reports; iii) facilitate the automatic distribution of images through departments [56].
Generally, every healthcare organization has a PACS which manages the various modes of digital image acquisition. A structured PACS comprises an image acquisition system and a secure network connecting radiology workstations (on-site or off-site) with a centralized archive [1]. The DICOM standard is used in order to simplify the interoperability of different devices in acquisition, transmission and saving of images.
Digital Imaging and Communications in Medicine (DICOM) was developed by the American College of Radiology and the National Electrical Manufacturers’ Association [57], in order to use fully digital images with high resolution instead of physical X-ray films [58].
DICOM is an international standard for all clinical images and relevant metadata and concerns the handling, storing, printing and transmitting phases [59], [60]. This standard allows to manage different types of medical images with other data such as: patient name, reference number, study number, dates and reports [61].
The DICOM standard is widely adopted in radiology, cardiology and radiotherapy imaging, and it is progressively expanding in other medicinal areas, like ophthalmology and dentistry [62].
Health Level Seven (HL7) is another important standard which allows the standardisation of the exchange of electronic health information. It is focused on data communication and not on data storage and presents the following versions: HL7 v2, HL7 v3 and the most recent FHIR (Fast Healthcare Interoperability Resources) which uses real-time RESTful interfaces [1]. In particular, HL7 v2 is chosen from local hospital for the exchange of healthcare information, including electronic medical record information [63]. HL7 v3 is designed to be the successor to v2 and overcomes the v2’s shortcomings. Finally, FHIR combines the features of HL7 v2 and v3 with the modern web technologies such as the REST architecture, in order to facilitate its implementation [63], [64]. In particular, differently from v2, FHIR is not based on the exchange of messages when certain events occur but on the availability of data and information exposed through a server, defining in this way the Resources (patient, encounter, condition, observation, procedures, care plan, goal and appointment), which are organized into modules, each representing a different functional area.
Modules are structured in 3 groups and 5 levels: infrastructure (levels 1 and 2), content (levels 3 and 4) and reasoning (level 5) [65].
In order to support the adoption of international standards such as DICOM or HL7, a consortium of professionals and industries named Integrating the Healthcare Enterprise (IHE) has been defined. IHE preserves a list of domains such as cardiology, radiology, pharmacy, IT system and patient care. In this context, it is important to mention the Cross Enterprise Basic eReferral Workflow Definition Profile (XBER-WD), which defines and standardises the workflow related to an eReferral Document, the actors involved and the digital documents related with the process [66]. XBER-WD is a standard based on a document type called Cross-Enterprise Document Workflow (XDW), in which the tasks completed in the workflow, the inputs and the outputs are stored [1].
The XDW standard supports participants in a complex environment to track and manage tasks related to clinical workflows, providing a common interoperability infrastructure to support them. All the documents can be exchanged between organisations through Cross-Enterprise Document Sharing (XDS) repositories, which facilitate the registration, sharing and storage across health enterprises of the patient electronic health records, in order to associate documents containing medical data to a specific workflow [67], [68].
3. HINT project
The HINT (Healthcare INtegration in Telemedicine)[1] project aims to implement a clinical support network both in cases requiring high specialization and to cover areas without specific expertise. The project develops a platform for the management of cases requiring access to diagnostic images, with the possibility of applying specific medical expertise even when no one is physically present where the images are produced. Specifically, the project envisages the realization of technological solutions aimed at optimizing the communication between the multi-disciplinary teams involved in a clinical case. Research activities also focus on defining tools which improve clinical data collection and healthcare information management, as well as on the clinical workflow efficiency, supporting the Physician in the decision-making process. HINT aims to realise a multi-target approach by integrating Physician support with the suggestion of diagnostic pathways, relying on a computational architecture capable of managing large data sets and algorithms for process mining and deep learning [1].
The research topics addressed by the project concern innovation in the area of:
- Cloud architectures in the clinical health field;
- Clinical Decision Support Systems and Computer Aided Diagnosis systems;
- Deep Learning models and algorithms;
- Integration and management standards for clinical processes;
- Secure data storage.
3.1 The BPM approach and lifecycle applied to the project
Looking at the approaches used in recent years, it is possible to note that there have been health and telemedicine projects which have used Workflow Management Systems based on the Business Process Management (BPM) approach and on the Business Process Model and Notation (BPMN) [69]. The BPM and BPMN tools allow to optimize clinical processes, tracking the key health parameters of an individual patient, organizing and monitoring all the healthcare activities, in order to support health organizations [70], [71].
The business processes are intended as “logically related tasks performed to achieve a defined business outcome” [72]. The BPM approach embodies methods and technologies which enable organizations to analyse, manage and optimize business processes [1], [73].
In [74], the authors analyse three BPM lifecycle proposals: the BPM lifecycle defined by Van der Aalst, the BPM lifecycle proposed by Netjes, and the BPM lifecycle proposed by Weske.
The first author proposes the BPM lifecycle with four steps: i) process design; ii) system configuration; iii) process enactment; iv) diagnosis phase, concerning processes’ monitoring and analysis [75].
The second approach includes five steps: i) design; ii) configuration; iii) execution; iv) control; v) diagnosis, which provides information in order to identify opportunities for improvement, workflow bottlenecks and any other critical points [76].
The last approach presents a cycle consisting of the following four steps: i) design and analysis; ii) configuration; iii) enactment; iv) evaluation of the business processes’ performance [77].
Taking the cue from the models proposed, the lifecycle of the health processes managed in the project (starting from modelling to optimization) are described and shown in the following revised phases and in Figure 1 [1], [78]:
- Process analysis and modelling;
- Process implementation;
- Process execution;
- Process monitoring.
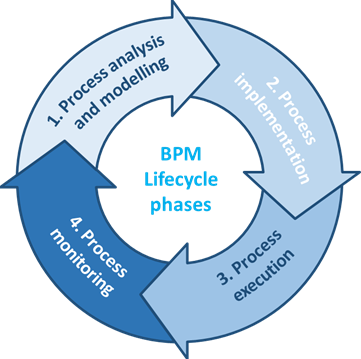
Figure 1: BPM lifecycle phases in HINT project
In the analysis phase, a business problem is highlighted and studied, in order to identify and analyse the related processes. The outcome of the process analysis is a new or updated process model which makes available a complete overview of the organization processes. In the modelling step, the current state of processes and the related activities are designed and modelled using tools and notations as BPMN, DMN (Decision Model and Notation), CMMN (Case Management Model and Notation) [1].
Then, in the implementation phase, the changes required to shift from the As-Is process to the To-Be process are defined and performed [63]. In particular, this phase involves two different aspects: the organizational change management and the process automation. Once the process has been mapped and illustrated, during the execution phase, it is run and tested, allowing its adaptation to the users’ needs. Then, a series of logs and measurements are collected and used in the monitoring phase, in order to analyse the process performance through specific Key Performance Indicators (KPI) and targets [1]. The notations mentioned above can be used for the process modelling: BPMN, CMMN and DMN, which can support the clinical process management.
In particular, an application example can be seen in [79], which recreates a guideline for stable ischemic heart disease, and considers the advantages and limitations of representing clinical pathways with these three notations. Moreover, [80] presents a clinical pathway for living donor liver transplantation using a combined approach which involves the event processing (BPMN) and the case management (CMMN) [81]. Another applicative case is presented in [82], which reports a study in healthcare sector, using DMN and BPMN approaches in an integrated manner, analysing a pediatric surgery process in a mid-size hospital. Finally, [83] combines the BPMN and DMN notations for modelling care pathways in a standardised manner.
As previously analysed, the BPM proved its usefulness to improve the design and therefore the telemedicine processes’ implementation. Indeed, there are some cases of the BPM application in the field of telemedicine projects, regarding, for example, de-hospitalization services with focus on e-Health solutions [84], or related to chronic pathologies such as Chronic Obstructive Pulmonary Disease (COPD) with a patient-centered approach based on telemedicine devices [85]. There is also a study concerning the use of the BPM methodology in healthcare with reference to the end-user interaction with EHR interface [86], as well as a study involving patients with hypertension whose healthcare processes are modelled using the BPM paradigm in order to identify weaknesses and mitigate them, for a better patient empowerment [87]. These studies underline that BPM applied to telemedicine is an efficient approach which can improve the management of the all-internal processes, the work of healthcare operators, with a positive impact on the quality of care and life of the patients.
In fact, in recent years, different clinical organisations have applied a BPM-based technology approach in order to improve the process management in healthcare sector.
In this way the quality and efficiency of processes can be increased, ensuring a better and continuous relationship with the patient. The use of BPM can also support medical practices by monitoring care processes, managing and analysing the clinical workflow and specific activities. A structured knowledge of the business context could be useful for the analyst in these activities [88], [89].
Table 1 summarizes and describes the BPM lifecycle phases in telemedicine processes, outlines the possible actors involved (Physicians, Specialists, Developers, Analysts) and identifies the clinical profiles, the standards (i.e. HL7, IHE, DICOM) and notations for process modelling and rule management [1].
Table 1 – BPM lifecycle phases, with related actors and clinical standards applied in the HINT project
| BMP Lifecycle | Description | Actors | Standards |
| 1. Business process analysis and modelling | The phase involves the identification and study of the relevant business processes and the As-Is process definition |
Business/Process Analyst Clinical domain experts (General Practitioner, Specialist, Healthcare Manager) |
BPMN CMMN DMN |
| 2. Business process implementation | The phase involves changes preparation needed to move from the As-Is process to the To-Be process in terms of process automation and management |
Software Developer Process Developer
|
CDA HL7 DICOM XBER-WD (IHE) XDS (IHE) DSUB (IHE) |
| 3. Business process execution | The phase involves To-Be process running and testing, with measurements and logs collection needed in the monitoring phase |
Physician and Specialist Users RIS/PACS systems DSS UWB devices |
DICOM XDW (IHE) FHIR |
| 4. Business process monitoring | The phase involves the collection of relevant data in order to define the process performance in relation to its KPIs |
Clinical Data Analyst Clinical Risk Manager
|
XDW (IHE) AUDIT LOG |
3.2 HINT architecture
The HINT project intends to develop a cloud platform with Hub and Spoke architecture for telemedicine based on imaging, which, by using international standards (DICOM, HL7, IHE), allows the integration of processes, health data and diagnostic images [1].
The cloud platform developed includes components which support Physicians and healthcare workers in the clinical cases management, enabling them to authenticate and authorise users, to manage roles, to search and consult the patient list, to manage examinations, to consult documents in the patient medical record, to open a clinical case, to record data in the required formats and to initiate and manage predefined diagnosis and treatment paths through the Workflow Manager functions whose interrelations will be highlighted later.
The core components developed, and described below, are: Portal, Hub and Spoke applications to manage Telemedicine services, DSS (Decision Support System), Workflow Management System, ESB (Enterprise Service Bus), VA (Virtual Archive) (Figure 2).
These components ensure [1]:
- user access to the different applications;
- the availability of basic record management services;
- access to integration services, allowing messages to be converted into the standard formats used in the health field;
- access to the necessary terminology management services;
- standard access to document archiving services.
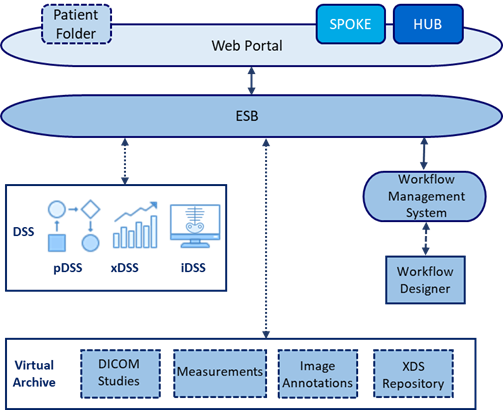
Figure 2 – HINT project architecture components
Portal
The HINT Portal provides the general services of the platform.
It consists of a web interface hosting all the user applications (Web Container), such as the Patient Folder, the agenda management, the visit management, etc. and allows access to the specific applications for Hub and Spoke telemedicine processes described in the scenarios.
The Portal allows basic consultation to the patient medical record, in which it is possible to examine the patient’s documents, the active pathways and the visit management through acceptance and discharge procedures.
The Portal offers a layer of back-end services to the other applications of the platform and has a local archiving component.
This layer mainly offers:
- Single Sign-On services (SSO);
- services for the univocal patient data management (Master Patient Index) and for the patients’ identification;
- EHR services.
Spoke
The Spoke represents a set of platform applications which enable the implementation of specific functionalities of a particular clinical-health task. Basically, a Spoke application identifies, for a requesting structure, the hardware and software equipment used to digitally record and archive the patient’s physiological data, documents and clinical studies, i.e. to make use of that set of information to perform the task and obtain a diagnosis. For HINT, Spoke functionality also includes the generation of requests for examinations and consultations (Neuro-Radiological and Dermatological teleconsultation).
The Spoke hardware and software equipment can be represented by a specific software application and by the following devices: medical devices (including UWB devices – Ultra Wide Band), diagnostic apparatus, RIS/PACS system.
Hub
The Hub represents a set of applications of the platform which allows to receive the notification and proceed to the completion of a particular clinical-health task. Basically, a Hub application identifies, for the supplying structure, the system used to consult data, documents and images and to record the diagnosis in a medical report. The Hub may be the display component of a teleconsultation, telemonitoring or teleassistance system, or even a RIS/PACS system.
ESB
The integration services of the HINT platform enable communication between the different components by sorting and transforming messages into formats supported by the final components.
The Enterprise Service Bus (ESB) component implements services dealing with the exchange of information between the front-end of the Portal together with the user applications (including Hub and Spoke) and the back-end components of the platform.
These services implement, when required, the transformation of the messages sent by the clients in JSON (XML format) for data and documents, and in JPEG format, for images, into the health standard formats (HL7, CDA, DICOM).
DSS
The Decision Support System (DSS) component allows the following activities: feature extraction; image classification and diagnostic support by means of a neural network (iDSS); diagnostic logs analysis for the identification of the diagnostic process patterns (pDSS); control of physiological data and alerts reporting (xDSS) [1].
Workflow Management System
The Workflow Management System is responsible for managing the execution of clinical processes modelled in BPMN, which comply with the specifications of the workflow definition profile standard defined by XBER-WD and for the storage of workflow documents in the XDS.
The Workflow Management System consists of these sub-systems:
- Workflow Engine and related services;
- Workflow Document Management and storage system.
The Workflow Engine manages the execution of processes and controls activities involving actors and applications. It receives communications which allow tasks to be updated through services compliant with the FHIR standard. Moreover, it manages the assignment of tasks, the progress of processes and the notifications to external components.
Virtual Archive
The Virtual Archive implements repository services for archiving clinical-health data, documents and images. The VA defines a unique interface layer for the portal and identifies the applications which need to archive data and documents generated during the execution of the processes supported by the platform.
4. HINT telemedicine processes
4.1 Neuro-Radiological Teleconsultation
This process describes the remote consulting activity between Physicians (Requesting Physicians and Clinical Specialists) who, being in two different places, can communicate with each other via ICT systems. In the specific case, the specialized organization (Hub), where the Clinical Specialist provides health services, gives, when required, medical consultations to the local organization (Spoke), which has available clinicians providing only some basic health services.
The principal activity regards the evaluation of the patient’s condition for first or second opinion by a Clinical Specialist, based on shared diagnostic images and clinical reports.
The entire process can be divided into the following phases [1]:
- Creation of a Referral Request;
- Consultation Scheduling;
- Clinical data control and evaluation by the Clinical Specialist (creation of report).
The HINT portal can manage the initial step concerning the admission of the patient to the clinical organization, the acquisition of the exam reports (MRI, PET, CT, diagnostic tests) carried out and the subsequent neurological evaluation during the first control visit. If the Requesting Physician of the Spoke Organization needs to perform a neuroradiology consultation by contacting the Hub Clinical Specialist, he/she can use the HINT system based on a workflow engine to create a Teleconsultation Referral Request. The Requesting Physician enters all the data regarding the teleconsulting request in the first free Hub.
The data to be entered in order to define the Request are: the patient’s personal data, request type (e.g., first neuro-radiological control, diagnostic valuation for second opinion), clinical history (e.g. trauma, potential stroke, dementia), urgency level, the list of past clinical exams (reports and digital images).
The Scheduling task creates a list of Hub structures (and related Clinical Specialists) which can take charge of the teleconsultation execution. The Requesting Physician can then select one of them from the list. A decision table based on specific rules (for example Physician specialization, his/her time-sheet and available days and times, intervention mode type) will create the list of potential Hub organizations which can take responsibility for the clinical services. The request is repeated until the referral has been assigned and executed by the available Hub.
When the Hub organization takes charge of the teleconsultation request, the Clinical Specialist performs the consultation and sends the file reference containing the diagnosis and the related report. If the Hub does not take charge of the request within a predefined time interval based on the case urgency, it is sent to another organization. The Clinical Specialist can acquire and display all the patient’s data and information regarding his/her clinical case.
After a thorough study of the specific case, the Clinical Specialist provides his/her consultation by first or second opinion. The Spoke application which has started the process receives a notification of final diagnosis, so the related Requesting Physician can analyse the consultation report provided by the colleague [1]. The BPMN model of the teleconsultation process, realised with the open-source Signavio software, is represented in Figure 3 and Figure 4, the latter represents the related sub-process.
4.2 Dermatological Teleconsultation
The periodic check of the moles is fundamental for prevention and early detection of the presence of any skin cancers or melanomas, and it can improve significantly the chances of cure. In fact, early diagnosis is an important factor to treat this type of skin pathologies in time.
Another teleconsultation process analysed and implemented in the project, regards specifically the melanoma pathologies, which is similar to the one described for the neuro-Radiological teleconsultation. In fact, the process steps are based on these phases: Dermatological image acquisition, Request for teleconsultation referral and its Scheduling, in order to find a specific Dermatology Clinical Specialist and the clinical evaluation through artificial neural network with the final report.
In this process, the platform must acquire the patient’s data in order to perform analyses through a neural network and to provide predictions referring to the type of skin lesions and related statistics.
Unlike the previous scenario, a DSS is used by the Dermatology Clinical Specialist to support the evaluation of the clinical situation. It is focused on the analysis of images assimilated in previous diagnostic cases of melanoma. The imaging DSS (iDSS) is based on specific images fingerprint extraction (features) and it permits a diagnostic image classification through the neural network [1].
The application can acquire all biometrics data (phenotype, ethnicity), personal data (region and province of residence, age, sex) and dermoscopic images (png, jpeg, jpg or DICOM) of a patient. In this way, it is possible to carry out analyses based on these data through a neural network, to return the predictions referred to the typology of the cutaneous lesions and to characterize any melanomas.
In this clinical scenario, the Spoke Requesting Physician visits the patient and enters in the platform all his/her personal data and past clinical information (exams reports, dermatological images). The Requesting Physician may indicate the diagnosis regarding the specific case, if the clinical situation is clear after the first visit.
If necessary, the Requesting Physician can send a teleconsultation request to the Dermatology Clinical Specialist of a Hub for a first opinion (when the initial diagnosis has not been made and the case is sent to the Dermatology Clinical Specialist immediately) or for a second opinion after the diagnosis. The Dermatology Clinical Specialist who takes over the case can be supported in his/her analyses by a neural network which can:
- request the prediction of specific skin pathology evaluation returned as the most likely disease class;
- check the 5 similar cases retrieved from the dataset and compared with the image linked to the patient.
In this way, the Requesting Physician is supported in detecting the presence of possible melanomas. Thanks to the neural network (DSS), the Dermatology Clinical Specialist has the opportunity to compare the new dermoscopic images acquired regarding the suspected lesions or moles of a patient with those present in the system dataset. A comparison is then made to identify any similarities and consequently to provide the Requesting Physician with specific classes and coefficients of cosine similarity (fingerprints comparison).
The steps of the Dermatology Clinical Specialist for the evaluation of a clinical case via neural network and 5 similar cases are:
- the Dermatology Clinical Specialist selects the clinical case for which he/she wants to obtain a prediction regarding the acquisitions of data and images he/she has made;
- the neural network returns the predicted class with the probabilities of all other similar classes;
- the Dermatology Clinical Specialist can also request the 5 most similar acquisitions;
- the neural network returns the 5 images acquisition having the greatest correspondence with the patient’s image, in order to be evaluated on the basis of a coefficient of similarity.
The Requesting Physician may use the results provided by the system to write the Dermatology Clinical Specialist diagnosis regarding the selected clinical case. In addition, statistics can be extracted by analysing biometric and personal data using DSS techniques. Also in this scenario, the Spoke organization which has initiated the process, receives a notification of completed diagnosis made by the Hub organization. The BPMN model of the dermatological teleconsultation process is represented with the open-source Signavio software in Figure 5 and Figure 6, the latter represents the related sub-process.
4.3 Telemonitoring – OSAS Syndrome Diagnosis
This process analyses the telemonitoring of the patient’s heart and respiratory rate during sleep time to diagnose the Obstructive Sleep Apnoea Syndrome (OSAS). The system uses a non-invasive Ultra-Wide Band (UWB) technology, thanks to which it is possible to acquire data related to the patient’s heart and breathing rate during sleep time in a non-invasive way.
The Physician of a health organization (public or private hospital) forwards the request for sleep monitoring in order to analyse the clinical situation of the patient, while a specific health operator of the Hub/Spoke assigned to the service, responds to this request. The service can also be provided at patient’s home by activating a monitoring system based on digital devices. This home system is able to acquire, in contactless mode, clinical data from the patient during sleep. In addition, there is a tablet acting as a gateway, which receives the recorded data from the UWB device and retransmits them to the system [1].
The processes for this telemonitoring case are basically two and both involve the Physicians, the Clinical Specialists, the healthcare operators and the patients as follows:
- the diagnosis formulation based on sleep data collected in a predefined period;
- the subsequent real-time sleep telemonitoring finalized to continue the evaluation of the clinical case over time.
Formulation of diagnosis by telemonitoring
The steps of the first process leading to the formulation of the diagnosis by telemonitoring and to the subsequent report definition are specified below:
- Creation of pre-diagnosis sleep telemonitoring request;
- Receiving pre-diagnosis telemonitoring request;
- Configuration and installation of sleep telemonitoring kit;
- Start and end of data collection;
- Sleep monitoring data recovery for the patient;
- Diagnosis and report formulation.
After the request has been sent, the system assigns the task to the most suitable Hub/Spoke operator, who can manage the activity and supervise the process until its conclusion, with the production of the final report by the Hub Clinical Specialist.
The Physician who started the telemonitoring request, can recover the patient’s monitoring data in order to evaluate his/her clinical condition. In the first phase regarding the Pre-diagnosis, the initial clinical information about the patient’s condition and the data collected from the monitoring for a given time interval (time series of hearth and breath rate) are recorded in the local database and indicated as reference model to the patient.
After this monitoring phase, the Clinical Specialist can examine the patient’s pattern to diagnose the eventual Obstructive Sleep Apnoea Syndrome and produce the associated report which will be saved in the system. Once the diagnosis has been defined, the Physician, consulting with the Clinical Specialist, can decide to perform a successive telemonitoring phase to record the patient’s sleep apnoea episodes for an extended period. If further telemonitoring activity is not necessary, the Physician communicates the final diagnosis to the patient (Figure 7 and Figure 9, the latter represents the related sub-process) [1].
Telemonitoring and real-time evaluation
If the patient is afflicted with OSAS or the Physician needs to further investigate the patient’s clinical situation, he/she can decide to set up a telemonitoring process, in order to control the evolution of the medical case in a medium or long period.
In this second scenario (Figure 8 and Figure 9, the latter represents the related sub-process), the activities regarding the telemonitoring and real-time evaluation are defined. They are aimed at detecting any critical situation on the basis of clinical data acquired which show a deviation from normal values (reference pattern) and, consequently, provide indications for a timely intervention and a possible change of care plan.
The steps of this second process are:
- Telemonitoring plan definition;
- Creation of sleep telemonitoring request;
- Receiving of telemonitoring request;
- Telemonitoring kit configuration;
- Start of telemonitoring activities and data collection;
- Data processing from xDSS;
- Management of possible alert sent to the system and their visualization by the Physician;
- Control phase for a possible extension of telemonitoring service at the end of the predefined period;
- Final clinical evaluation by the Specialist.
In this situation, there is an initial phase of telemonitoring programme definition, followed by its subsequent referral to the Hub/Spoke operator, who then configures the telemonitoring kit.
After the telemonitoring process has been defined and started, the real time data collected from the patient’s UWB device, with the standard model data collected during the pre-diagnosis monitoring, are given as input to the platform’s xDSS. The xDSS allows the analysis of patient data from the activated monitoring and, in case of significant deviations between the data collected in the pre-diagnosis and the data acquired through real-time telemonitoring, an alert message is sent by the system to the deputy Physicians. In this way, the system processes the real-time data and compares them with the patient’s standard pattern, promptly notifying the presence of its deviation, such as an ongoing night apnoea episode [1]. The potential alert generated by the platform can, then, be viewed and managed by the Physician. At the end of the process, the Specialist makes an assessment of the OSAS data from the telemonitoring and makes it available and viewable to the requesting Physician.
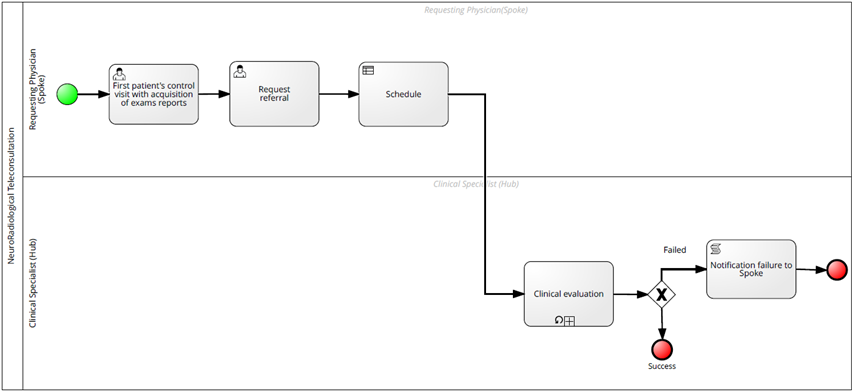
Figure 3 – NeuroRadiological Teleconsultation
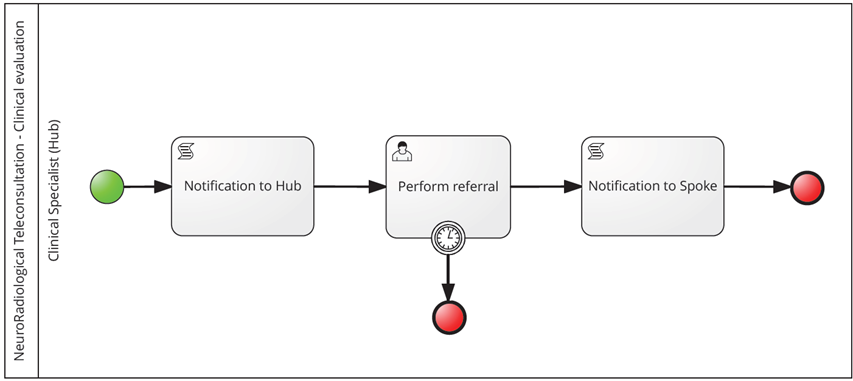
Figure 4 – NeuroRadiological Teleconsultation Subprocess: Clinical evaluation
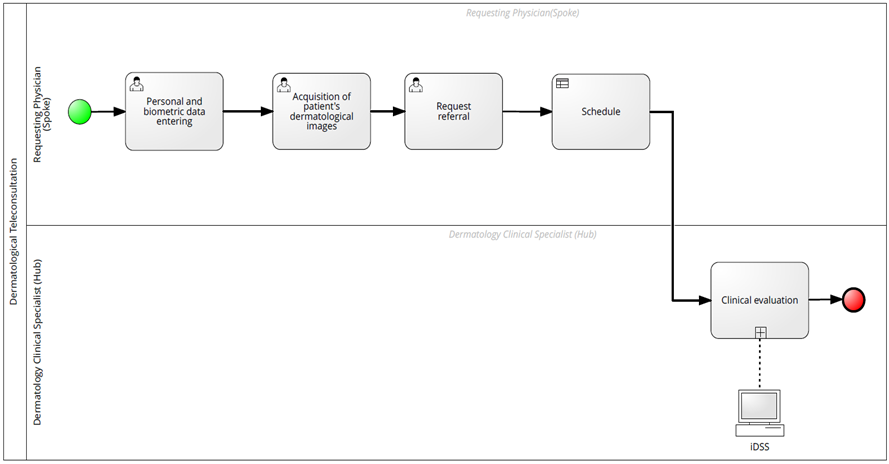
Figure 5 – Dermatological Teleconsultation
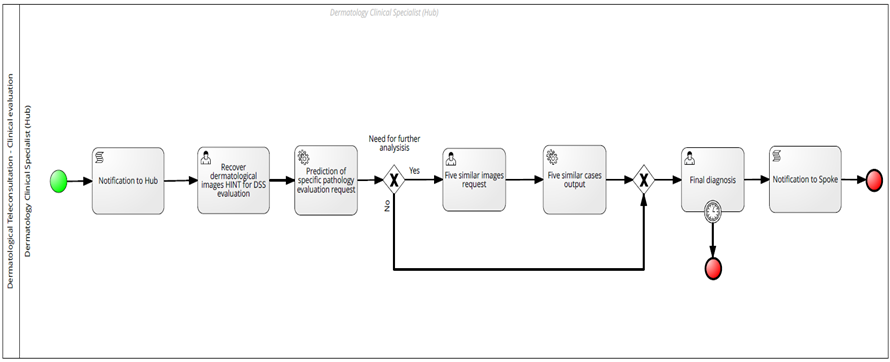
Figure 6 – Dermatological Teleconsultation Subprocess: Clinical evaluation
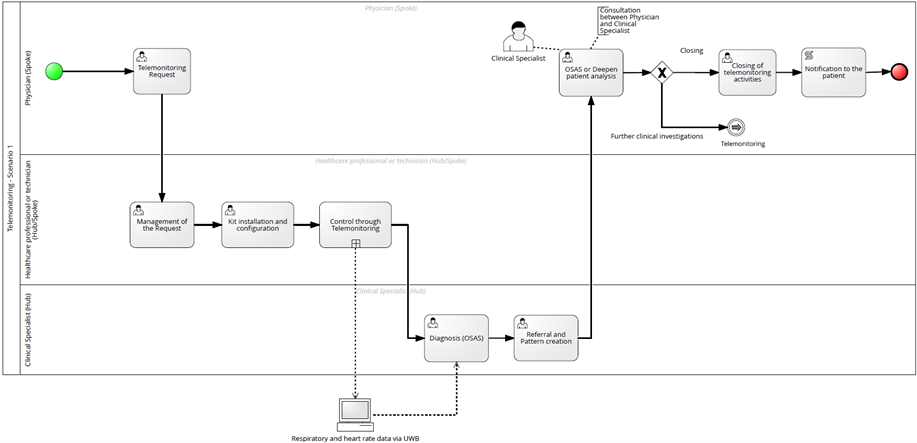
Figure 7: Telemonitoring process – Scenario 1
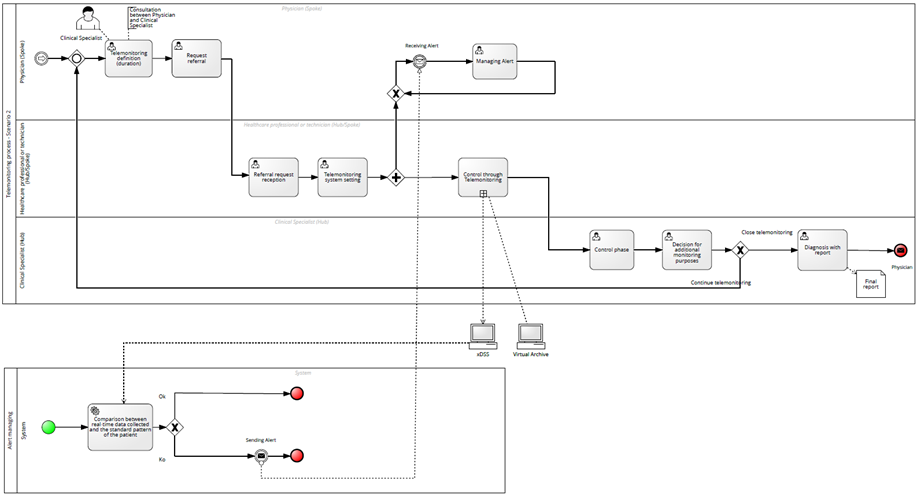
Figure 8 – Telemonitoring process – Scenario 2
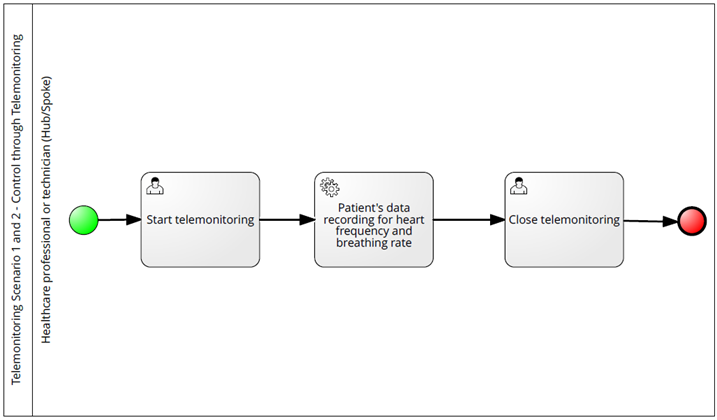
Figure 9 – Telemonitoring process Subprocess: Control through telemonitoring
5. Discussion and Conclusions
The use of telemedicine systems, supported by an efficient territorial health service, can reduce the number of admissions and inappropriate hospitalization, making home monitoring and treatments more effective [90]. This approach can allow a better interaction with Specialists and an accurate control of patients’ clinical situation through the use of medical IoT devices.
The HINT project fits perfectly this context, as it has provided a comprehensive and optimized framework based on a flexible and workflow-focused teleconsultation and telemonitoring platform.
The new Hub and Spoke architecture proposed in this project allow Physicians (Hub) to find Specialists (Spoke) for a consultation even in remote areas, where medical specialists are not physically present, thanks to innovative teleradiology, teleconsultation and telemonitoring solutions.
An important innovation in the HINT project concerned the introduction of a Decision Support System for dermatological teleconsultation within a cloud telemedicine platform, which allows the classification of dermoscopic images of skin lesions, thanks to Artificial Intelligence and Deep Learning techniques.
Another important innovation, in the field of Obstructive Sleep Apnoea Syndrome, concerned the introduction of advanced monitoring devices.
Moreover, a workflow management component within the HINT platform, based on BPM, allowed the automated management of the clinical processes’ activities and related data sharing. The steps of the BPM lifecycle were implemented specifying, for each phase, the healthcare standards used and the actors involved, in order to re-engineer the clinical processes analysed (see Table 1).
The technological and organisational innovations led to the definition of a prototype, whose components and functionalities have been tested but not in a real clinical setting. However, the HINT technological applications have been successfully used in the Italian LHA (Local Health Authority) by some partners after the project conclusion.
Many potential advantages deriving from HINT telemedicine solutions, involve different end-users. In particular, Physicians can be supported in finding the most suitable patient’s diagnostic process, through telemonitoring and telehealth appointments.
Furthermore, in emergency situations, telemedicine can represent a guidance for Specialist Consultants (SPs) and for hospital admission, since, thanks to telemonitoring systems combined with possible teleconsultations with other Physicians, it is possible to know the patient’s clinical situation before he/she arrives at the hospital. For private or public healthcare organisations, telemedicine systems can give the possibility to ensure an effective coverage of the largest number of clinical cases as well as a service homogeneity offered on the territory, thanks to the support of integrated platforms enabling advanced care systems. The support in the diagnosis phase through IT systems based on telemedicine services can help the Specialist Physicians, who can work also remotely in a more efficient and effective way [1].
The advantages for patients can concern the availability of more specialist services within the hospital or territory healthcare processes. They can also benefit from the empowerment process ensured by telemedicine services, thanks to which they can be more involved in their diagnosis processes and in healthcare treatments.
Finally, using telemedicine systems, patients can reduce time and costs needed to get efficient medical care.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The research was supported by the Apulia Region and Italian Ministry of Economic Development within the Innonetwork Call (POR 2014-2020 – FESR Funds, Axis I, Action 1.6), project HINT (Healthcare INtegration in Telemedicine) number 7ZKNZM4 – CUP: B37H17002850007. The authors also acknowledge the contributions of all the project partners to the definition of healthcare scenarios and to the development of the HINT platform.
- A. Caforio, T. Calogiuri, M. Lazoi, G. Mitrano, R. Paiano, “HINT project: a BPM teleconsultation and telemonitoring platform”, in Proceedings of the 10th International Conference on Information Systems and Technologies, Lecce Italy, 1–8, 2020. doi: 10.1145/3447568.3448542.
- A.V. Gaddi, F. Cascini, E. Chiarolla, B. Delfrate, S. Forti, M. Marchetti, “Telemonitoraggio e telecontrollo per i cittadini con malattie cardiologiche, respiratorie e diabete”, MONITOR, 47, 21–26, 2022.
- J. Wiegel, B. Seppen, M. van der Leeden, M. van der Esch, R. de Vries, W. Bos, “Adherence to Telemonitoring by Electronic Patient-Reported Outcome Measures in Patients with Chronic Diseases: A Systematic Review”, IJERPH, 18(19), 2021, doi: 10.3390/ijerph181910161.
- D. Voran, “Telemedicine and beyond”, Mo Med, 112(2), 129–135, 2015.
- I. Khemapech, W. Sansrimahachai, M. Toahchoodee, “Telemedicine – Meaning, Challenges and Opportunities”, Siriraj Med Bull, 71(3), 246–252, 2019, doi: 10.33192/Smj.2019.38.
- J. Adler, C. Yu, M. Datta, “The changing face of radiology: from local practice to global network”, Medical Journal of Australia, 190(1), 20–23, 2009, doi: 10.5694/j.1326-5377.2009.tb02256.x
- C.L. Snoswell, M.L. Taylor, T.A. Comans, A. C. Smith, L.C. Gray, L.J. Caffery, “Determining if Telehealth Can Reduce Health System Costs: Scoping Review”, J Med Internet Res, 22(10), 17298, 2020, doi: 10.2196/17298.
- E.B. Allely, “Synchronous and asynchronous telemedicine”, J Med Syst, 19(3), 207–212, 1995, doi: 10.1007/BF02257174.
- M. Batool, A. Jalal, K. Kim, “Telemonitoring of Daily Activity Using Accelerometer and Gyroscope in Smart Home Environments”, J. Electr. Eng. Technol., 15(6), 2801–2809, 2020, doi: 10.1007/s42835-020-00554-y.
- D. Dias, J. Paulo Silva Cunha, “Wearable Health Devices—Vital Sign Monitoring, Systems and Technologies”, Sensors, 18(8), 2414, 2018, doi: 10.3390/s18082414.
- A. Rosotti, Informatica medica. Sistemi informativi sanitari e reti di telemedicina. McGraw-Hill Education, 2021.
- ACR Data Science Institute, “ACR DSI and Standards Bodies Active in Artificial Intelligence Space”, ACR DATA SCIENCE INSTITUTE, American College of Radiology.
- A.K. Gupta, A. Garg, M.S. Sandhu, “Diagnostic radiology: advances in imaging technology, Third edition”, Medical Publishers, 2019.
- R. Nuzzi, P. Marolo, A. Nuzzi, “The Hub-and-Spoke Management of Glaucoma”, Front. Neurosci, 14, 180, 2020, doi: 10.3389/fnins.2020.00180.
- T. Chong et al., “The California Telepathology Service: UCLA’s Experience in Deploying a Regional Digital Pathology Subspecialty Consultation Network”, Journal of Pathology Informatics, 10(1), 31, 2019, doi: 10.4103/jpi.jpi_22_19.
- G. Boland, J.T. Schlakman, J.H. Thrall, “Teleradiology”, in PACS, K. J. Dreyer, J.H. Thrall, D.S. Hirschorn, e A. Mehta, A c. di New York: Springer-Verlag, 523–560, 2006, doi: 10.1007/0-387-31070-3_26.
- E.R. Ranschaert, F.H.B. Binkhuysen, “European Teleradiology now and in the future: results of an online survey”, Insights Imaging, 4(1), 93–102, 2013, doi: 10.1007/s13244-012-0210-z.
- B. Horn, D. Chang, J. Bendelstein, J.C. Hiatt, “Implementation of a Teleradiology System to Improve After-Hours Radiology Services in Kaiser Permanente Southern California”, TPJ, 10(1), 47–50, 2006, doi: 10.7812/TPP/05-119.
- R.S. Lewis, J.H. Sunshine, M. Bhargavan, “Radiology Practices’ Use of External Off-Hours Teleradiology Services in 2007 and Changes Since 2003”, American Journal of Roentgenology, 193(5), 1333–1339, 2009, doi: 10.2214/AJR.09.2984.
- H. Eklöf, E. Radecka, P. Liss, “Teleradiology uppsala–sydney for nighttime emergencies: preliminary experience”, Acta Radiol, 48(8), 851–853, 2007, doi: 10.1080/02841850701422120.
- A. Kalyanpur, J. Weinberg, V. Neklesa, J.A. Brink, H.P. Forman, “Emergency radiology coverage: technical and clinical feasibility of an international teleradiology model”, Emergency Radiology, 10(3), 115–118, 2003, doi: 10.1007/s10140-003-0284-5.
- A. Martinon et al., “Teleradiology saves times in cases of vital emergencies: A comparative study with on-call radiology in two urban medium-sized French hospitals”, European Research in Telemedicine / La Recherche Européenne en Télémédecine, 3(4), 151–160, 2014, doi: 10.1016/j.eurtel.2014.10.001.
- T.C.M. Pechet, G. Girard, B. Walsh, “The value teleradiology represents for Europe: A study of lessons learned in the U.S.”, European Journal of Radiology, 73(1), 36–39, 2010, doi: 10.1016/j.ejrad.2009.10.019.
- C. Eakins et al., “Second Opinion Interpretations by Specialty Radiologists at a Pediatric Hospital: Rate of Disagreement and Clinical Implications”, American Journal of Roentgenology, 199(4), 916–920, 2012, doi: 10.2214/AJR.11.7662.
- E. Zan, D.M. Yousem, M. Carone, J.S. Lewin, “Second-Opinion Consultations in Neuroradiology”, Radiology, 255(1), 135–141, 2010, doi: 10.1148/radiol.09090831.
- H.K. Huang, “Teleradiology technologies and some service models”, Computerized Medical Imaging and Graphics, 20(2), 59–68, 1996, doi: 10.1016/0895-6111(96)00032-8.
- G.A. Naqvi, M. Daly, A. Dawood, A. Kurkuri, S. Kutty, “Smart consultation for musculoskeletal trauma: Accuracy of using smart phones for fracture diagnosis”, The Surgeon, 12(1), 32–34, 2014, doi: 10.1016/j.surge.2013.09.001.
- F.J. Kammerer, M. Hammon, P.M. Schlechtweg, M. Uder, S.A. Schwab, “A web based cross-platform application for teleconsultation in radiology”, J Telemed Telecare, 21(6), 355–363, 2015, doi: 10.1177/1357633X15575237.
- J.H. Thrall, “Teleradiology Part I. History and Clinical Applications”, Radiology, 243(3), 613–617, 2007, doi: 10.1148/radiol.2433070350.
- A. Bonnin, “Medical tele-imaging: a good chance for the future”, Bull Acad Natl Med, 183(6), 1123–1134, 1999.
- K. Deldar, K. Bahaadinbeigy, “Teleconsultation and Clinical Decision Making: a Systematic Review”, Acta Inform Med, 24(4), 286, 2016, doi: 10.5455/aim.2016.24.286-292.
- S. Conway, “Teleradiology and telemedicine: They are not equal”, Managing Quality, Safety, and Cost in Radiology, and Learning to Wear it Well, 28–29, 2016.
- Sanitanova, “Concept Hub & Spoke”, Monitor dolore – Sanitanova..
- M. Skorning et al., “Teleconsultation in pre-hospital emergency medical services: Real-time telemedical support in a prospective controlled simulation study”, Resuscitation, 83(5), 626–632, 2012, doi: 10.1016/j.resuscitation.2011.10.029.
- C. Chandhanayingyong, B. Tangtrakulwanich, T. Kiriratnikom, “Teleconsultation for emergency orthopaedic patients using the multimedia messaging service via mobile phones”, J Telemed Telecare, 13(4), 193–196, 2007, doi: 10.1258/135763307780908049.
- H. Bourdon et al., “Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: Experience with 500 patients in March and April 2020”, Journal Français d’Ophtalmologie, 43(7), 577–585, 2020, doi: 10.1016/j.jfo.2020.05.005.
- G. Pare, M. Jaana, C. Sicotte, “Systematic Review of Home Telemonitoring for Chronic Diseases: The Evidence Base”, Journal of the American Medical Informatics Association, 14(3), 269–277, 2007, doi: 10.1197/jamia.M2270.
- S. Crossen, N. Glaser, H. Sauers-Ford, S. Chen, V. Tran, J. Marcin, “Home-based video visits for pediatric patients with poorly controlled type 1 diabetes”, J Telemed Telecare, 26(6), 349–355, 2020, doi: 10.1177/1357633X19828173.
- K.L. Margolis et al., “Effect of Home Blood Pressure Telemonitoring and Pharmacist Management on Blood Pressure Control: A Cluster Randomized Clinical Trial”, JAMA, 310(1), 46, 2013, doi: 10.1001/jama.2013.6549.
- R. Bellazzi et al., “A telemedicine support for diabetes management: the T-IDDM project”, Computer Methods and Programs in Biomedicine, 69(2), 147–161, 2002, doi: 10.1016/S0169-2607(02)00038-X.
- B. Morlion, C. Knoop, M. Paiva, M. Estenne, “Internet-based Home Monitoring of Pulmonary Function after Lung Transplantation”, Am J Respir Crit Care Med, 165(5), 694–697, 2002, doi: 10.1164/ajrccm.165.5.2107059
- C. Maiolo, E.I. Mohamed, C.M. Fiorani, A. de Lorenzo, “Home telemonitoring for patients with severe respiratory illness: the Italian experience”, J Telemed Telecare, 9(2), 67–71, 2003, doi: 10.1258/135763303321327902.
- N.B. Shah, E. Der, C. Ruggerio, P.A. Heidenreich, B.M. Massie, “Prevention of hospitalizations for heart failure with an interactive home monitoring program”, American Heart Journal, 135(3), 373–378, 1998, doi: 10.1016/S0002-8703(98)70310-2.
- G. Labarca et al., “Efficacy of continuous positive airway pressure (CPAP) in patients with obstructive sleep apnea (OSA) and resistant hypertension (RH): Systematic review and meta-analysis”, Sleep Medicine Reviews, 58, 101446, 2021, doi: 10.1016/j.smrv.2021.101446.
- C. Chen, J. Wang, L. Pang, Y. Wang, G. Ma, W. Liao, “Telemonitor care helps CPAP compliance in patients with obstructive sleep apnea: a systemic review and meta-analysis of randomized controlled trials”, Therapeutic Advances in Chronic Disease, 11, 2020, doi: 10.1177/2040622320901625.
- C. Turino et al., “Management of continuous positive airway pressure treatment compliance using telemonitoring in obstructive sleep apnoea”, Eur Respir J, 49(2), 1601128, 2017, doi: 10.1183/13993003.01128-2016.
- N. Fox et al., “The Impact of a Telemedicine Monitoring System on Positive Airway Pressure Adherence in Patients with Obstructive Sleep Apnea: A Randomized Controlled Trial”, Sleep, 35(4), 477–481, 2012, doi: 10.5665/sleep.1728.
- E. Seto, K.J. Leonard, J.A. Cafazzo, J. Barnsley, C. Masino, H.J. Ross, “Developing healthcare rule-based expert systems: Case study of a heart failure telemonitoring system”, International Journal of Medical Informatics, 81(8), 556–565, 2012, doi: 10.1016/j.ijmedinf.2012.03.001.
- S. Wali et al., “Expanding Telemonitoring in a Virtual World: A Case Study of the Expansion of a Heart Failure Telemonitoring Program During the COVID-19 Pandemic”, J Med Internet Res, 23(1), 2021, doi: 10.2196/26165.
- World Health Organization, WHO global report on falls prevention in older age. Geneva, Switzerland: World Health Organization, 2008.
- H. Eren e J.G. Webster, Telemedicine and electronic medicine. Boca Raton: CRC Press, Taylor & Francis Group, 2016.
- S.K. Boell, D. Cecez-Kecmanovic, “What is an Information System?”, in 2015 48th Hawaii International Conference on System Sciences, HI, USA, 4959–4968, 2015. doi: 10.1109/HICSS.2015.587.
- A.R. Bakker, “HIS, RIS, and PACS”, Computerized Medical Imaging and Graphics, 15(3), 157–160, 1991, doi: 10.1016/0895-6111(91)90004-F.
- T. Nakamura, H. Hitsuishi, T. Harada, “Cooperation between the Hospital Information System and the File Maker Pro”, in 2007 IEEE/ICME International Conference on Complex Medical Engineering, Beijing, China, 291–294, 2007. doi: 10.1109/ICCME.2007.4381741.
- B. Mansoori, K.K. Erhard, J.L. Sunshine, “Picture Archiving and Communication System (PACS) Implementation, Integration & Benefits in an Integrated Health System”, Academic Radiology, 19(2), 229–235, 2012, doi: 10.1016/j.acra.2011.11.009.
- S. Boochever, “HIS/RIS/PACS integration: getting to the gold standard”, Radiology management, 26(3), 16–24, 2004.
- M. Gupta, N. Singh, K. Shrivastava, P. Mishra, “Significance of digital imaging and communication in medicine in digital imaging”, Digit Med, 1(2), 63, 2015, doi: 10.4103/2226-8561.174769.
- M. Hosseini, B.E. Dixon, “Syntactic Interoperability and the Role of Standards”, in Health Information Exchange, Elsevier, 123–136, 2016, doi: 10.1016/B978-0-12-803135-3.00008-6.
- I.D. McLean, J. Martensen, “Specialized Imaging”, in Clinical Imaging, Elsevier, 44–78, 2014, doi: 10.1016/B978-0-323-08495-6.00002-6.
- M. Licurse, W. Boonn, Computers in radiology, 26, 2016.
- R. Bibb, D. Eggbeer, A. Paterson, Medical modelling: the application of advanced design and rapid prototyping techniques in medicine, Second edition. Amsterdam Boston Cambridge Heidelberg: Elsevier/ Woodhead Publishing, 2015.
- M.M. Cruz-Cunha, I.M. Miranda, P. Goncalves, Handbook of research on ICTSs and management systems for improving efficiency in healthcare and social care. Hershey PA: Medical Information Science Reference, 2013.
- D. Bender, K. Sartipi, “HL7 FHIR: An Agile and RESTful approach to healthcare information exchange”, in Proceedings of the 26th IEEE International Symposium on Computer-Based Medical Systems, Porto, Portugal, 326–331, 2013, doi: 10.1109/CBMS.2013.6627810.
- R. Noumeir, “Active Learning of the HL7 Medical Standard”, J Digit Imaging, 32(3), 354–361, 2019, doi: 10.1007/s10278-018-0134-3.
- M. Mangia, “Alla scoperta di FHIR”, Salute digitale, 2022.
- Integrating the Healthcare Enterprise, IHE Patient Care Coordination (PCC) Technical Framework, 1, 2016.
- Integrating the Healthcare Enterprise, IT Infrastructure (ITI) Technical Framework, 1, 2022.
- A. Sakellarios, “A cloud-based platform for the non-invasive management of coronary artery disease”, Enterprise Information Systems, 14(8), 1102–1123, 2020, doi: 10.1080/17517575.2020.1746975.
- P. Szmodics, “Evaluating the organizational knowledge based on business process management”, PhD, Corvinus University of Budapest, Budapest, 2018. doi: 10.14267/phd.2018020.
- A. Capodieci, G. Del Fiore, L. Mainetti, “Adopting Collaborative Business Processes To Prevent The Loss Of Information In Public Administration Organisations”, 2014, doi: 10.5281/ZENODO.1092317.
- U. Barchetti, A. Capodieci, A. L. Guido, L. Mainetti, “Information Systems for Knowledge Workers: The Kpeople Enterprise 2.0 Tool”, in Web Information Systems Engineering – WISE 2012, X. S. Wang, I. Cruz, A. Delis, e G. Huang, A c. di Berlin, Heidelberg: Springer Berlin Heidelberg, 7651, 804–807, 2012, doi: 10.1007/978-3-642-35063-4_71.
- T. Davenport, J. Short, The new Industrial Engineering: Information Technology and Business Process Redesign. 2015.
- P. Harmon, Business process change: a guide for business managers and BPM and six sigma professionals, 2nd ed. Amsterdam ; Boston: Elsevier/Morgan Kaufmann Publishers, 2007.
- R. Macedo de Morais, S. Kazan, S. Inês Dallavalle de Pádua, A. Lucirton Costa, “An analysis of BPM lifecycles: from a literature review to a framework proposal”, Business Process Management Journal, 20(3), 412–432, 2014, doi: 10.1108/BPMJ-03-2013-0035.
- W.M.P. van der Aalst, “Business Process Management Demystified: A Tutorial on Models, Systems and Standards for Workflow Management”, in Lectures on Concurrency and Petri Nets, 3098, Springer Berlin Heidelberg, 1–65, 2004, doi: 10.1007/978-3-540-27755-2_1.
- M. Netjes, H.A. Reijers, W.M.P. Van der Aalst, “Supporting the BPM life-cycle with FileNet”, EMMSAD, 135–146, 2006.
- M. Weske, Business process management: concepts, languages, architectures, 2nd ed. Berlin, Springer, 2012.
- M. Dumas, M. La Rosa, J. Mendling, H.A. Reijers, Fundamentals of business process management. Berlin: Springer, 2015.
- J. Chae, B.H. Park, M. Jones, M. Ward, J. Nebeker, “Converting Clinical Pathways to BPM+ Standards: A Case Study in Stable Ischemic Heart Disease”, in 2020 IEEE 33rd International Symposium on Computer-Based Medical Systems (CBMS), Rochester, MN, USA, 453–456, 2020, doi: 10.1109/CBMS49503.2020.00092.
- N. Herzberg, K. Kirchner, M. Weske, “Modeling and Monitoring Variability in Hospital Treatments: A Scenario Using CMMN”, in Business Process Management Workshops, F. Fournier e J. Mendling, A c. di Cham: Springer International Publishing, 202, 3–15, 2015, doi: 10.1007/978-3-319-15895-2_1.
- C. Combi, B. Oliboni, A. Zardini, F. Zerbato, “A Methodological Framework for the Integrated Design of Decision-Intensive Care Pathways—an Application to the Management of COPD Patients”, J Healthc Inform Res, 1(2), 157–217, 2017, doi: 10.1007/s41666-017-0007-4.
- A. Bianchi, M. Mortari, C. Pintavalle, G. Pozzi, “Putting BPMN and DMN to Work: a Pediatric Surgery Case Study”, in 2021 IEEE International Conference on Digital Health (ICDH), Chicago, IL, USA, 154–159, 2021, doi: 10.1109/ICDH52753.2021.00028.
- I. Essefi, H.B. Rahmouni, M.F. Ladeb, “Integrated privacy decision in BPMN clinical care pathways models using DMN”, Procedia Computer Science, 196, 509–516, 2022, doi: 10.1016/j.procs.2021.12.043.
- E. Sulis et al., “Monitoring patients with fragilities in the context of de-hospitalization services: An Ambient Assisted Living Healthcare Framework for e-Health applications”, in 2019 IEEE 23rd International Symposium on Consumer Technologies (ISCT), Ancona, Italy, 216–219, 2019, doi: 10.1109/ISCE.2019.8900989.
- M. Szelągowski, J. Berniak-Woźny, C. Lipiński, “BPM Support for Patient-Centred Clinical Pathways in Chronic Diseases”, Sensors, 21(21), 7383, 2021, doi: 10.3390/s21217383.
- J. Gomes, F. Portela, M.F. Santos, “Introduction to BPM approach in Healthcare and Case Study of End User Interaction with EHR Interface”, Procedia Computer Science, 141, 519–524, 2018, doi: 10.1016/j.procs.2018.10.132.
- D. Ruiz-Fernández, D. Marcos-Jorquera, V. Gilart-Iglesias, V. Vives-Boix, J. Ramírez-Navarro, “Empowerment of Patients with Hypertension through BPM, IoT and Remote Sensing”, Sensors, 17(10), 2273, 2017, doi: 10.3390/s17102273.
- A. Caione, A.L. Guido, A. Martella, R. Paiano, A. Pandurino, “Knowledge base support for dynamic information system management”, Inf Syst E-Bus Manage, 14(3), 533–576, 2016, doi: 10.1007/s10257-015-0294-3.
- R. Paiano, A. Caione, “A Knowledge Base Guided Approach for Process Modeling in Complex Business Domain”, in Proceedings of the 11th International Joint Conference on Software Technologies, Lisbon, Portugal, 169–176, 2016, doi: 10.5220/0005974801690176.
- N.D. Brunetti, S. Scalvini, G. Molinari, “Innovations in telemedicine for cardiovascular care”, Expert Review of Cardiovascular Therapy, 14(3), 267–280, 2016, doi: 10.1586/14779072.2016.1140572.
