A Structuration View of the South African National Health Insurance Readiness
Volume 7, Issue 6, Page No 174-180, 2022
Author’s Name: Nomawethu Tungela, Tiko Iyamua)
View Affiliations
Department of Informatics and Design, Cape Peninsula University of Technology, Cape Town, +27, South Africa
a)whom correspondence should be addressed. E-mail: connectvilla@yahoo.com
Adv. Sci. Technol. Eng. Syst. J. 7(6), 174-180 (2022); ![]() DOI: 10.25046/aj070618
DOI: 10.25046/aj070618
Keywords: National health insurance, Readiness assessment, Structuration theory, South Africa
Export Citations
The South African government has embarked on the implementation of the National Health Insurance (NHI), to increase access to healthcare and improve service delivery. However, the project has being encountering various challenges, which are not empirically known. The aim of the study is to identify the factors that influence the implementation of the NHI from ICT readiness assessment perspective. Qualitative data was collected from communities and healthcare service providers including government as the legislative body. The duality of structure of structuration theory was used as lens to guide the analysis of the study, from ICT readiness assessment and perspective. From the analysis, four factors, current state, areas of coverage, role of ICT, role of human are found to influence the implementation of the NHI. The originality of the findings lies on the empirical nature of the study.
Received: 02 August 2022, Accepted: 03 November 2022, Published Online: 20 December 2022
1. Introduction and Background
Many people in some countries including South Africa have limited access to quality healthcare services [1]. The lack or limited access to healthcare services can be attributed to factors such as exorbitant costs, lack of available or not enough professional healthcare personnel and insufficient healthcare facilities. This leads to inequalities in the use of the healthcare services in many parts of the world [2]. With the increase of inequalities that are faced by the healthcare sector there is a demand for higher accessibility of quality service rendered to the citizens especially in the rural or peri-urban communities. According to [3], peri-urban areas are areas “which have some initial features and functionality of cities but are not yet defined as cities, including the rural–urban interface, small town, township and village”. To ensure that these demands are met the World Health Organization (WHO) has made a recommendation for countries to employ the universal health coverage (UHC) [4].
In support and alignment with the UHC, the South African government has introduced the National Health Insurance (NHI), which requires Information and Communication Technology (ICT) in its implementation. The NHI is intended to provide extended access and improved quality of healthcare services across the country. In essence, the NHI system is primarily aimed at bridging the gap between the lower income earners and the middle class by providing equal healthcare services to all citizens [2]. However, how ready the environment is unknown, at least, from empirical perspective. The term readiness “is related to terms such as ‘innovation’ and ‘adoption’ of new technologies” [5]. Assessment is referred to the collection of information on how things are done in an organization [6].
The newness of the NHI requires the South African environment to be ready for its implementation. This is primarily to avoid failure like many other initiatives, which can be a serious catastrophe for the government and the citizens that look forward to its benefits. Over the years, many systems have failed because of factors such as lack of infrastructures [5]. Traditional affiliation and culture of an environment have also been instrumental factors to the success and failure of many systems [7]. From these viewpoints it is essentially important to assess the readiness of a diverse environment like South Africa before critical systems such as the NHI can be implemented, particularly in the rural areas of the country.
The South African NHI makes provision for ease of access to healthcare services irrespective of socio-economic status [8]. Significantly, the NHI is expected to be of benefit. [9] argue that many health fatalities are due to factors such as the waiting period to access healthcare services and insufficient skilled healthcare practitioners. According to [10], private health services are prohibitive, which results to limited access by many citizens. Hence, [11] suggest that benefits of having access to health insurance include reduced cost and ease of access. However, implementation of the NHI requires understanding of its readiness in the South African environment.
2. Review of literature
This section presents the review of literature focusing on Information and Communication Technology (ICT), healthcare, National Health Insurance (NHI), readiness assessment.
Information and Communication Technology (ICT) has been widely used in the health sector in many different countries. ICT makes it easier and possible for the patients and service providers including government to provide and receive healthcare services [12]. According to [13], there has been a solid development on how ICT is being used in the healthcare sector to improve on service delivery. Through ICT, patients’ records are remotely monitored, and medical records are electronically stored [14]. Hence, according to [15], ICT in developing countries has been considered as the principal technology for advancement of quality patient care in healthcare. This is due to its ability to bring change in service delivery especially in the healthcare sector [16].
The use of ICT has seen the birth of many services like e-health which according to [7] are “noticeable on the development of the healthcare sector in developing countries”. According to [17], healthcare practitioners can communicate by using their mobile devices such as smart phones to provide healthcare services. In addition, local governments in many countries have made major investment in the ICT infrastructure so that the citizens can receive excellent, efficient healthcare services [18]. Moreover, the innovations that are brought by ICT can bring about change in a way that patients are being diagnosed and monitored [19].
The Universal Health Coverage (UHC) is all about ensuring that all citizens have access to the quality health services they need with minimum contributions [20], which the South African NHI system tries to align with. According to [10], it can also ensure the availability of sufficient resources that are effective. [21] claimed that UHC is only achieved when all citizens of the country receive good health services without financial burden. Furthermore, [22] defined UHC as having equal access of healthcare services amongst all citizens to overcome the differences of the health system. According to [4] “Universal coverage is determined by how much government budget can be allocated to subsidise premiums for poor and low-income families and informal sector workers”. To fully achieve the goal of UHC, all citizens of the country should have universal access to the services that are provided by the healthcare.
There is an increasing failure in the implementation of new systems or policies in many organizations including the healthcare sector due to lack of readiness [23]. Various factors such as infrastructure and skill set influences readiness, which should be known and understood before embarking on implementation of new systems [24]. According to [5], readiness assessment is a mechanism for minimising risks and possible failures. Readiness assessment is a tool for supporting service delivery in the healthcare because it identifies the gaps and interventions needed. As stated by [25], readiness assessment is concerned with how the healthcare facilities can deliver basic services at lower standards.
3. Structuration theory
Based on the objectives of the study which concerns factors such as rules, resources, different agents (or agencies), and the relationship between these factors, the structuration theory was selected to underpin the study. Structuration theory, according to [26] is a theory that focuses on social systems with technical enablement. The theory was introduced by Anthony Giddens in 1984 and had since been used in many research fields, including Information Technology (IT) to underpin studies for many years [27]. According to [28], the structuration theory has two main tenets which are (i) structure and (ii) agency, which are the core parts of its duality of structure as shown in Figure 1 below.
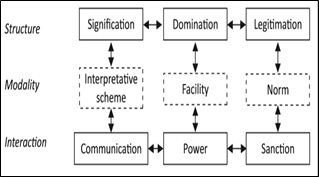
Figure 1: Duality of Structure [27]
According to [29], the structure consists of signification, domination and legitimation. The modality according to [28] consists of the interpretative scheme, facility and norm, and according to [30] the interaction comprises of communication, power and sanction. The author furthermore claims that modality provides the connection between the structure and the interaction of the agencies. Interaction amongst agencies is communicated through the interpretive schemes which are common knowledge that agencies use to interpret events by giving them meaning that demands signification structure [29]. The actions of agencies are made based on the ability to exercise power, using the facilities which are resources to obtain domination structure. The conduct of agencies becomes sanctioned or approved and end-up produces norm which results in the legitimation structure [31].
The structuration theory according to [32] can be used as a lens to enable the researcher to view and interpret data collected. Moreover, [28] claim that the structuration theory has been identified as a theory that is most suitable to interpret the results of the research. According to [29] the structure of the theory is made up of two properties which are rules and resources, and the agency of the theory according to [31] is made up of human and non-human agents. According to [29] the interactions which people make in a social process are constructed from the structures (rules and resources), from which interaction, new rules and resources are formed. The author furthermore claims that this iterative formation of rules and resources by peoples’ actions are commonly known as the duality of structure.
4. Research Methodology
We employ the discourse technique to analyze the traces in the views that led to the ideological and believe of individuals and groups about NHI in South Africa. The discourse approach seeks to identify hegemony and emancipate marginalized individuals and ideas [33]. Using the technique, it allows us to draw from interpretive paradigms [34], meaning we could employ our judgments and subjectivity as explained by [35].
The discourse technique is often applied to analyze within context, to understand the meanings that are associated with object through the process of communication and how it influences mobilization [36]. In the context of this study, the discourse technique allows us to gain insights into how the citizens understand the deployment of NHI in the country, using the radio as a platform to engage and dialogue with citizens. The technique enables tracing of connections between object and subject in a discourse [33].
Table 1: Duality of structure as lens for analysis
| # | Level | Duality of structure | Description |
| 1 | Macro conversation |
Structure
|
to gain insight on how NHI is understood from social and health contexts in individual’s real-life situation. This was structured into attributes, themes, and patterns relevant to the research, from both IT and non-IT related issues. |
|
Modality
|
|||
| Interaction | |||
| 2 | Micro reflectivity |
Structure
|
Individual’s communicative motivation informs the selection of linguistic forms, which influence conversation and meanings associated with the subject (He, 2017). Follows the interplay in the communicative motivation about views on NHI deployment. |
|
Modality
|
|||
| Interaction | |||
| 3 | Link between the micro and macro components |
Structure
|
Enables reflexivity consideration of how individuals and groups worldviews [35] of the NHI in South Africa. Links the micro and macro views, to reflexively examine our subjective understanding of the views. |
|
Modality
|
|||
| Interaction |
5. Assessing the South African NHI for Readiness
As shown in Table 1, the duality of structure from the perspective of structuration theory is used as a lens, to view the empirical evidence was viewed and answers to the questions were obtained: what is the current state of NHI implementation? presented to answer the question. The duality of structure presented the current state of the implementation of the NHI system in the communities of the country. From the signification structure, the importance of the implementation of the NHI system as the system that promotes access to quality healthcare services for all the citizens of the country. As the South African government communicate regarding this new system the citizens used their stock of knowledge to consider whether what has been communicated was important or not.
In assessing the readiness of the South African NHI for readiness, two fundamental factors were the focus: (1) on macro level, the importance is viewed; and (2) on micro level, the implications of not conducting assessments in the deployment of the concept were examined. Finally, the macro (importance) and micro (implications) were linked, to gain better insight of the current state and factors that influence readiness of the South African NHI, from IT perspective. At the macro level, the following question was used to the determinant: What is the current state of the implementation of the NHI? The question, what are the factors that can enable or constrain the NHI readiness? was used to examine the influencing factors from a micro level perspective.
5.1. What is the current state of the implementation of the NHI?
From ICT perspective, the current situation leans on two factors, access to health and area of coverage. The factors motivate, at the same time constrain the implementation of the NHI in the country. The factors contribute to the criticality of assessment of the South African NHI before implementation.
Access to healthcare
Currently, there are challenges in accessing healthcare services in the country. The challenges come from both technical and non-technical factors. [37] claim that it is vital to invest in an IT infrastructure to better the health facilities and increase access services in a country. The health sector on its own struggle to improve the quality and access to healthcare services, which negatively affect health of the citizens of the country. According to [20], this has prompted external stakeholders, such as the government and other sectors, to get involved in some countries. According to [38] lack of infrastructure can influence the effectiveness and efficiency of healthcare services delivered to the citizens. [39] assert that encouragement of healthcare personnel and the use of modern technology in healthcare facilities can better the health service delivery.
A successful implementation of the NHI makes it mandatory for the South African government to have a centralised database where patient records can be stored [40]. According to [37] central storage of records assist the health system between different healthcare personnel in different healthcare facilities to respond in real-time. This is because healthcare personnel can retrieve reports on the system through patient history [25]. However, there are many challenges with the current state of healthcare services and facilities. Two of the predominantly challenges are of technical and non-technical nature.
From the technical perspectives, some of the challenges are security. Security is referred to an act of prohibiting unlicensed users to gain access into an organization’s network [41]. Security is also a necessity when medical practitioners share patient data to other service providers [42]. Moreover, [43] assert that data security is needed even when the data is stored. Waiting times are also problematic. The technical challenges heavily contribute to successful implementation of the NHI through healthy readiness assessment [44].
Non-technical factors include availability of skilled healthcare personnel and healthcare infrastructure [25]. This assists the healthcare sector to be able to compare if the existing health resources will be able to stand the requirements to provide the NHI [45]. In India it was found that due to unskilled healthcare personnel the level of incorrect treatment issued was high [44]. Authors continue to claim that the only solution to mitigate the challenges is to continuously check and evaluate new avenues of that specific challenge. Moreover, [46] suggest that to successfully manage the existing challenges, there needs to be continuous planning and management within the healthcare sector.
Area of Coverage
The aim of the NHI is to provide high standard of healthcare services that will be available to all the citizens of the country irrespective of their geographic area [38]. [47] argues that there is still a large gap that exists between the urban and the rural areas of the country in terms of accessing and making use of the healthcare services available. [48] claim that “Expansion of coverage to poor and vulnerable populations often needs strong governmental commitment to give voice to marginalised groups and overcome interest-group politics”. This is because in any country that has a united political structure within its government, changes are easily accepted [49].
However, some of the challenges identified in the areas of coverage and access above are not unique to South African. For example, some of the challenges hindered similar programmes to the extent; they were either unsuccessful or terminated in many countries, such as Cyprus [50]. In some countries, there were over expenditure of budget due to implementation challenges [37], which can be attributed to lack of readiness assessment. The USA is an example, where, from inception Obamacare was faced with challenges where citizens were unable to register on its web-based system which left many citizens of the country unable to renew their insurance policies [51]. In Korea, health data have been encrypted so that it can be protected from unauthorised users. In Taiwan all the citizens of the country have been given a unique personal identification, this is to ensure privacy when they access their health information online [37].
5.2. What are the factors that can enable or constrain the NHI readiness?
As revealed from the analysis, primarily, two factors enable and at the same constrain the implementation of the NHI in South Africa. The factors are ICT and humans, which play fundamental roles from both technical and non-technical perspectives. Primarily, the factors require the need to continuously evolute the technology solutions and, training and development of ICT and healthcare personnel. The factors have the capability to enable and constrain the readiness of the phenomenon. [30] argues that factors enable and at the same time constrain processes and activities in IT projects. Thus, the factors are significant in a sense that it ensures that the various stakeholders adhere to the tasks and processes in the implementation and support of the NHI. Also, factors of influence can happen consciously or unconsciously [27], at both technical and non-technical structural levels during implementation.
Additionally, the factors, ICT and humans enable the integration of healthcare processes with technology solutions of different healthcare facilities, ensuring compatibility. The rationale for this is that the systems will be flexible and accommodate new and old systems when sharing data in an organization. This also ensures the efficiency and the effectiveness of service delivery that is needed in the healthcare sector. Lastly, the factor which is governance and controls plays a big role in the implementation of the NHI. The implication of mismanagement of funds can affect the objective of the organization and can result in the failure of the implementation of the NHI system. With strict policies and accountability this can be minimized.
The Role of ICT
The implementation of the NHI in any government including South Africa, requires the use of ICT as it assists in the improvement of the quality and effectiveness of health service delivery [52]. Daily, the healthcare sector deals with large volumes of data such as sensitive patient information e-Health is defined as the service where the healthcare sector uses ICT to deliver services such as treating patients and monitoring diseases [53]. In addition, [54] suggest that the use of electronic data systems as opposed to the traditional paper-based system can improve the efficiency of medical practitioners.
Many governments around the world including South Africa continuously look at the ways they can use ICT, to better their healthcare services [55]. However, according to [56] healthcare in South Africa is faced with challenges such as poor infrastructure and lack of funds. Another challenge according to [57] is the lack of privacy and security which poses a threat to sensitive healthcare data.
The role of humans
Healthcare personnel are the ones that have an obligation for the implementation of the NHI in South Africa [58]. [59] argue that for the NHI to be successfully implemented in South Africa, the key role players such as medical practitioners in service delivery within the healthcare sector needs to be involved. However, [60] argue that many people around the country including healthcare personnel are not enlightened about the concept of the NHI and that is due to insufficient communication shared so far. On the other hand, [61] suggest that the government and the Department of Health need to take serious measures to have consultation with communities, to spread the word about the NHI system. [62] claim that requirements such as sufficient human resources need to be achieved simultaneously with the implementation of the NHI.
5.3. Link between importance and implication of implementing the NHI
The macro level allows acknowledgment of how institutional contexts differ in their enabling and constraining influence [63], which makes it useful in classifying the activities and action of the various stakeholders. The macro level helps to maintain inferences at group levels of analysis [64]. Linking the macro and the micro perspectives, is purposely to obtain a comprehensive view [65], on how factors influence and constrain NHI activities at individual and facilities’ levels.
Currently, there are challenges in accessing healthcare services in the country. The challenges come from both technical and non-technical factors, which reveal significance and implications in coverage, the role of ICT, and the role of humans. The technical factors include security [66] and data storage [67]. Some of these challenges are contextual, meaning that they must be customized for individual environments. Thus, the same measure cannot be used for two countries, because they often differ in infrastructural, cultural and governmental settings [68], hence, readiness assessment is required.
The NHI system can be successfully implemented in the communities of the country, guided by the influencing factors, to understand the processes and activities better. This includes managing relationship between the factors. Critically, this is intended to guide the interaction between the human-to-human, human-and -technology, and technology-and-technology that are involved in the implementation of the NHI. Through the practical application of the influencing factors, government can become more knowledgeable during and post implementation of the NHI.
6. Conclusion
The influencing factors identified in this study will be of significance to the stakeholders involved in the implementation of the NHI in South Africa, from both technical and non-technical perspectives. The factors are expected to boost the strength and capability of the relevant authorities with knowledgeable power to employ the resources, in implementing the NHI, in providing healthcare services to the community.
The study has been thoroughly carried out following the research methodology as stated in the section above. This includes the use of structuration theory as a lens, which brings rigor to the study. The significance of the study is through the development of the framework which can be of great assistance to the South African government and governments from other countries if followed. The framework can provide guidance on how an ICT system can be implemented for service delivery. The South African government, department of health and other governments from developing countries will benefit from this empirical study in three-fold, theoretically, methodologically and practically. Theoretically as the study will contribute to the existing theory through the addition to the body of knowledge, methodological based on the philosophies, approaches, methods and techniques that will be followed or employed on the study and practically on the basis that the researcher has developed the framework which will serve as a guide to help governments to better understand processes to be taken before implementation of the new system.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgment
The authors would like to thank IT department in Cape Peninsula University of Technology for the support.
- I. Garcia-Subirats, I. Vargas, A.S. Mogollón-Pérez, P. De Paepe, M.R.F. da Silva, J.P. Unger, M.L. Vázquez, “Barriers in access to healthcare in countries with different health systems. A cross-sectional study in municipalities of central Colombia and north-eastern Brazil,” Social science & medicine, 106, 204-213, 2014, doi:10.1016/j.socscimed.2014.01.054.
- L. Mhlaba, D. Blaauw, A. Parry, “Is National Health Insurance a viable option for South Africa? Experiences from other countries,” AfricaGrowth Agenda, 2016(10), 8-12, 2016.
- L. Tian, B. Ge, Y. Li, “Impacts of state-led and bottom-up urbanization on land use change in the peri-urban areas of Shanghai: Planned growth or uncontrolled sprawl?,” Cities, 60, 476-486, 2016, doi:10.1016/j.cities.2016.01.002.
- W.C. Hsiao, S.H. Cheng, W. Yip, “What can be achieved with a single-payer NHI system: The case of Taiwan,” Social Science & Medicine, 233, 265-271, 2019, doi:10.1016/j.socscimed.2016.12.006.
- S. Adjorlolo, G. Ellingsen, “Readiness assessment for implementation of electronic patient record in Ghana: a case of university of Ghana hospital,” Journal of Health Informatics in Developing Countries, 7(2), 128-140, 2013.
- A.N Hidayanto, M.A. Hasibuan, P.W. Handayani, Y.G. Sucahyo, “Framework for Measuring ERP Implementation Readiness in Small and Medium Enterprise (SME): A Case Study in Software Developer Company,” Journal of Computers, 8(7), 1777-1782, 2013, doi:10.4304/jcp.8.7.1777-1782.
- M.R. Hoque, M.F.A. Mazmum, Y. Bao, “e-Health in Bangladesh: current status, challenges, and future direction,” The International Technology Management Review, 4(2), 87-96, 2014, doi:10.2991/itmr.2014.4.2.3.
- J. Dixon, E.Y. Tenkorang, I.N. Luginaah, V.Z. Kuuire, G.O. Boateng, “National health insurance scheme enrolment and antenatal care among women in G hana: is there any relationship?,” Tropical Medicine & International Health, 19(1), 98-106, 2014, doi:10.1111/tmi.12223.
- A. Mills, “Health care systems in low-and middle-income countries,” New England Journal of Medicine, 370(6), 552-557, 2014, doi:10.1056/NEJMra1110897.
- I.A. Odeyemi, “Community-based health insurance programmes and the national health insurance scheme of Nigeria: challenges to uptake and integration,” International journal for equity in health, 13(1), 1-13, 2014, doi:10.1186/1475-9276-13-20.
- A. Brugiavini, N. Pace, “Extending health insurance in Ghana: effects of the National Health Insurance Scheme on maternity care,” Health economics review, 6(1), 1-10, 2016, doi:10.1186/s13561-016-0083-9.
- D. Haluza, D. Jungwirth, “ICT and the future of health care: aspects of health promotion,” International journal of medical informatics, 84(1), 48-57, 2015, doi:10.1016/j.ijmedinf.2014.09.005.
- H.K. Andreassen, L.E. Kjekshus, A. Tjora, “Survival of the project: a case study of ICT innovation in health care,” Social Science & Medicine, 132, 62-69, 2015, doi:10.1016/j.socscimed.2015.03.016.
- M.R. Cowie, J. Bax, N. Bruining, J.G. Cleland, F. Koehler, M. Malik, F. Pinto, E. van der Velde, P. Vardas, “e-Health: a position statement of the European Society of Cardiology,” European heart journal, 37(1), 63-66, 2016, doi:10.1093/eurheartj/ehv416.
- G. Fitzpatrick, G. Ellingsen, “A review of 25 years of CSCW research in healthcare: contributions, challenges and future agendas,” Computer Supported Cooperative Work (CSCW), 22(4), 609-665, 2013, doi:10.1007/s10606-012-9168-0.
- D. Haluza, D. Jungwirth, “ICT and the future of health care: aspects of pervasive health monitoring,” Informatics for Health and Social care, 43(1), 1-11, 2018, doi:10.1080/17538157.2016.1255215.
- A. Solanas, C. Patsakis, M. Conti, I.S. Vlachos, V. Ramos, F. Falcone, O. Postolache, P.A. Pérez-Martínez, R. Di Pietro, D.N. Perrea, et al, “Smart health: A context-aware health paradigm within smart cities,” IEEE Communications Magazine, 52(8), 74-81, 2014, doi:10.1109/MCOM.2014.6871673.
- J. Adler-Milstein, N. Sarma, L.R. Woskie, A.K. Jha, “A comparison of how four countries use health IT to support care for people with chronic conditions,” Health Affairs, 33(9), 1559-1566, 2014, doi:10.1377/hlthaff.2014.0424.
- C. Hollis, R. Morriss, J. Martin, S. Amani, R. Cotton, M. Denis, S. Lewis, “Technological innovations in mental healthcare: harnessing the digital revolution,” The British Journal of Psychiatry, 206(4), 263-265, 2015, doi:10.1192/bjp.bp.113.142612.
- L.O.M. de Andrade, A. Pellegrini Filho, O. Solar, F. Rígoli, L.M. de Salazar, P.C.F. Serrate, K.G. Ribeiro, T.S. Koller, F.N.B. Cruz, R. Atun, “Social determinants of health, universal health coverage, and sustainable development: case studies from Latin American countries,” The Lancet, 385(9975), 1343-1351, 2015, doi:10.1016/S0140-6736(14)61494-X.
- D.B. Evans, J. Hsu, T. Boerma, “Universal health coverage and universal access,” Bulletin of the World Health Organization, 91, 546-546A, 2013, doi:10.2471/BLT.13.125450 .
- G. Ooms, L.A. Latif, A. Waris, C.E. Brolan, R. Hammonds, E.A. Friedman, M. Mulumba, L. Forman, “Is universal health coverage the practical expression of the right to health care?,” BMC International Health and Human Rights, 14(1), 1-7, 2014, doi:10.1186/1472-698X-14-3.
- C.M. Shea, S.R. Jacobs, D.A. Esserman, K. Bruce, B.J. Weiner, “Organizational readiness for implementing change: a psychometric assessment of a new measure,” Implementation science, 9(1), 1-15, 2014, doi:10.1186/1748-5908-9-7.
- S. Khoja, H. Durrani, R.E. Scott, A. Sajwani, U. Piryani, “Conceptual framework for development of comprehensive e-health evaluation tool,” Telemedicine and e-Health, 19(1), 48-53, 2013, doi:10.1089/tmj.2012.0073.
- K. O’Neill, M. Takane, A. Sheffel, C. Abou-Zahr, T. Boerma, “Monitoring service delivery for universal health coverage: the Service Availability and Readiness Assessment,” Bulletin of the World Health Organization, 91, 923-931, 2013, doi:10.2471/BLT.12.116798.
- G. Puron-Cid, “Interdisciplinary application of structuration theory for e-government: A case study of an IT-enabled budget reform,” Government Information Quarterly, 30, S46-S58, 2013, doi:10.1016/j.giq.2012.07.010.
- A. Giddens, The constitution of society: Outline of the theory of structuration, University of California Press, 1984.
- A.F. Coad, L.G. Glyptis, “Structuration: a position–practice perspective and an illustrative study,” Critical Perspectives on Accounting, 25(2), 142-161, 2014, doi:10.1016/j.cpa.2012.10.002.
- C.L.H. Chang, “The interaction of political behaviors in information systems implementation processes–Structuration Theory,” Computers in Human Behavior, 33, 79-91, 2014, doi:10.1016/j.chb.2013.12.029.
- T. Iyamu, “Improvising information technology projects through the duality of structure,” South African Journal of Information Management, 19(1), 1-9, 2017, doi:10.4102/sajim.v19i1.797.
- H. Englund, J. Gerdin, “Structuration theory in accounting research: Applications and applicability,” Critical Perspectives on Accounting, 25(2), 162-180, 2014, doi:10.1016/j.cpa.2012.10.001.
- T. Iyamu, “Underpinning theories: Order of use in information systems research,” Journal of Systems and Information Technology, 15(3), 224-258, 2013, doi:10.1108/JSIT-11-2012-0064.
- C. Avgerou, C. Bonina, “Ideologies implicated in IT innovation in government: A critical discourse analysis of Mexico’s international trade administration,” Information Systems Journal, 30(1), 70-95, 2020, doi:10.1111/isj.12245.
- J.D. Wall, B.C. Stahl, A.F. Salam, “Critical discourse analysis as a review methodology: An empirical example,” Communications of the Association for Information Systems, 37(1), 257-285, 2015, doi:10.17705/1CAIS.03711.
- M.D. Myers, H.K. Klein, “A set of principles for conducting critical research in information systems,” MIS Quarterly, 35(1), 17-36, 2011, doi:10.2307/23043487.
- F. Shirazi, “Social media and the social movements in the Middle East and North Africa: A critical discourse analysis,” Information Technology & People, 26(1), 28-49, 2013, doi:10.1108/09593841311307123.
- T.M. Cheng, “Reflections on the 20th anniversary of Taiwan’s single-payer National Health Insurance System,” Health affairs, 34(3), 502-510, 2015, doi:10.1377/hlthaff.2014.1332.
- A. Fusheini, J. Eyles, “Achieving universal health coverage in South Africa through a district health system approach: conflicting ideologies of health care provision,” BMC Health Services Research, 16(1), 1-11, 2016, doi:10.1186/s12913-016-1797-4.
- S.R. Mishra, P. Khanal, D.K. Karki, P. Kallestrup, U. Enemark, “National health insurance policy in Nepal: challenges for implementation,” Global health action, 8(1), 28763, 2015, doi:10.3402/gha.v8.28763.
- S.O. Hynes, B. Pang, J.A. James, P. Maxwell, M. Salto-Tellez, “Tissue-based next generation sequencing: application in a universal healthcare system,” British Journal of Cancer, 116(5), 553-560, 2017, doi:10.1038/bjc.2016.452.
- K. Abouelmehdi, A. Beni-Hessane, H. Khaloufi, “Big healthcare data: preserving security and privacy,” Journal of big data, 5(1), 1-18, 2018, doi:10.1186/s40537-017-0110-7.
- A. Mouttham, C. Kuziemsky, D. Langayan, L. Peyton, J. Pereira, “Interoperable support for collaborative, mobile, and accessible health care,” Information systems frontiers, 14(1), 73-85, 2012, doi:10.1007/s10796-011-9296-y.
- J.A. Kim, S. Yoon, L.Y. Kim, D.S. Kim, “Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data,” Journal of Korean medical science, 32(5), 718-728, 2017, doi:10.3346/jkms.2017.32.5.718.
- C. Bredenkamp, T. Evans, L. Lagrada, J. Langenbrunner, S. Nachuk, T. Palu, “Emerging challenges in implementing universal health coverage in Asia,” Social science & medicine, 145, 243-248, 2015, doi:10.1016/j.socscimed.2015.07.025.
- A. Smith, J. Wishnia, D. Strugnell, S. Ranchod, “Human resources for health planning and National Health Insurance: the urgency and the opportunity,” South African health review, 2018(1), 23-31, 2018, doi:10.10520/EJC-14490f63b9.
- A. Edward, C. Branchini, I. Aitken, M. Roach, K. Osei-Bonsu, S.H. Arwal, “Toward universal coverage in Afghanistan: a multi-stakeholder assessment of capacity investments in the community health worker system,”Social science & medicine, 145, 173-183, 2015, doi:10.1016/j.socscimed.2015.06.011.
- L. Rispel, “Analysing the progress and fault lines of health sector transformation in South Africa,” South African health review, 2016(1), 17-23, 2016, doi:10.10520/EJC189322.
- M.R. Reich, J. Harris, N. Ikegami, A. Maeda, C. Cashin, E.C. Araujo, K. Takemi, T.G. Evans, “Moving towards universal health coverage: lessons from 11 country studies,” The Lancet, 387(10020), p811-816, 2016, doi:10.1016/S0140-6736(15)60002-2.
- J. Shiffman, “Political context and health financing reform,” Health Systems & Reform, 5(3), 257-259, 2019, doi:10.1080/23288604.2019.1633894.
- A. Polynikis, G. Lavranos, “Cyprus’ health system reform: Trials and tribulations,” Sağlık Akademisyenleri Dergisi, 5(1), 1-6, 2018, doi:10.5455/sad.13-1518617280.
- T. Rice, L.Y. Unruh, P. Rosenau, A.J. Barnes, R.B. Saltman, E. van Ginneken, “Challenges facing the United States of America in implementing universal coverage,” Bulletin of the World Health Organization, 92, 894-902, 2014, doi:10.2471/BLT.14.141762.
- M. Herselman, A. Botha, H. Toivanen, J. Myllyoja, T. Fogwill, R. Alberts, “A digital health innovation ecosystem for South Africa,” In 2016 IST-Africa Week Conference, 1-11, 2016, doi:10.1109/ISTAFRICA.2016.7530615.
- Y.C.J. Li, J.C. Yen, W.T Chiu, W.S. Jian, S. Syed-Abdul, M.H. Hsu, “Building a national electronic medical record exchange system–experiences in Taiwan,” Computer methods and programs in biomedicine, 121(1), 14-20, 2015, doi:10.1016/j.cmpb.2015.04.013.
- C.Y. Wright, M. Chersich, A. Mathee, “National Health Insurance and climate change: Planning for South Africa’s future,” South African Journal of Science, 115(9-10), 1-3, 2019, doi:10.17159/sajs.20169/5800.
- W. Raghupathi, V. Raghupathi, “Big data analytics in healthcare: promise and potential,” Health information science and systems, 2(1), 1-10, 2014, doi:10.1186/2047-2501-2-3.
- R. Pankomera, D. Van Greunen, P. Elizabeth, “December. Comparative analysis of the status of ICT usage in healthcare: South Africa, Tanzania, Malawi,” In Proceedings of the IASTED African Conference on Health Informatics (AfricaHI 2014), 2014, doi:10.2316/P.2014.815-021.
- T. Mgozi, R. Weeks, “December. The impact of cloud computing on the transformation of healthcare system in South Africa,” In 2015 ITU Kaleidoscope: Trust in the Information Society (K-2015), 1-7, 2015, doi:10.1109/Kaleidoscope.2015.7383636.
- S. Mndzebele, M. Matsi, “Perspectives and experiences of healthcare workers on the National Health Insurance at tertiary hospitals in the Limpopo Province, South Africa,” PULA: Botswana J Afr Stud, 30(1), 123-30, 2016.
- S. Latiff-Khamissa, P, Naidoo, “Knowledge, awareness and readiness of private sector doctors practising in the Ethekweni and Ugu districts of KwaZulu-Natal province for the implementation of the National Health Insurance,” South African Family Practice, 58(1), 18-23, 2016, doi:10.1080/20786190.2015.1123361.
- V.K. Molokomme, E. Seekoe, D.T. Goon, “The perception of professional nurses about the introduction of the National Health Insurance (NHI) in a private hospital in Gauteng, South Africa,” The Open Public Health Journal, 11(1), 234-242, 2018, doi:10.2174/1874944501811010234.
- G. Setswe, S. Muyanga, J. Witthuhn, P. Nyasulu, “Public awareness and knowledge of the National Health Insurance in South Africa,” Pan African Medical Journal, 22(1), 19-26, 2015, doi:10.11604/pamj.2015.22.19.6131.
- R. Pokharel, P.R. Silwal, “Social health insurance in Nepal: A health system departure toward the universal health coverage,” The International journal of health planning and management, 33(3), 573-580, 2018, doi.org/10.1002/hpm.2530.
- J. Van Wijk, C. Zietsma, S. Dorado, F.G. De Bakker, I. Marti, “Social innovation: Integrating micro, meso, and macro level insights from institutional theory,” Business & Society, 58(5), 887-918, 2019, doi:10.1177/0007650318789104.
- P.H. Kim, K. Wennberg, G. Croidieu, “Untapped riches of meso-level applications in multilevel entrepreneurship mechanisms,” Academy of Management Perspectives, 30(3), 273-291, 2016, doi:10.5465/amp.2015.0137.
- B. Wang, Q. Zhou, “Climate change in the Chinese mind: An overview of public perceptions at macro and micro levels,” Wiley Interdisciplinary Reviews: Climate Change, 11(3), e639, 2020, doi:10.1002/wcc.639.
- C. Esposito, A. De Santis, G. Tortora, H. Chang, K.K.R. Choo, “Blockchain: A panacea for healthcare cloud-based data security and privacy?,” IEEE Cloud Computing, 5(1), 31-37, 2018, doi:10.1109/MCC.2018.011791712.
- Y. Zhang, M. Qiu, C.W. Tsai, M.M. Hassan, A. Alamri, “Health-CPS: Healthcare cyber-physical system assisted by cloud and big data,” IEEE Systems Journal, 11(1), 88-95, 2015, doi:10.1109/JSYST.2015.2460747.
- V. Tangcharoensathien, A. Mills, T. Palu, “Accelerating health equity: the key role of universal health coverage in the Sustainable Development Goals,” BMC medicine, 13(1), 1-5, 2015, doi:10.1186/s12916-015-0342-3.
